What is Laparoscopic Cholecystectomy?
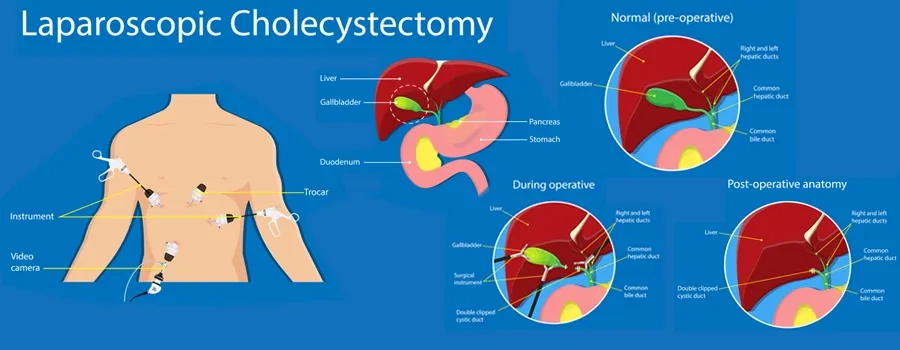
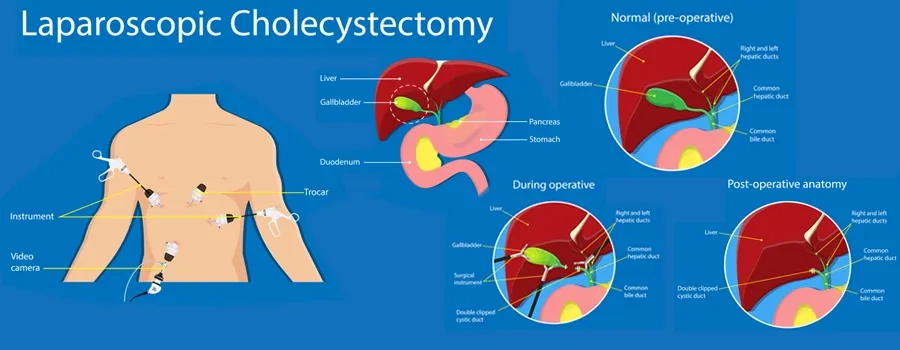
Laparoscopic cholecystectomy is a minimally invasive surgery used to remove the gallbladder, a small organ located under the liver that stores bile. It is the most common treatment for gallstones, gallbladder infections, and chronic gallbladder pain that does not improve with medication or lifestyle changes.
During the surgery, the surgeon makes a few tiny cuts in the abdomen and inserts a laparoscope (a thin tube with a camera) along with fine surgical instruments. The camera projects clear images onto a screen, guiding the surgeon in safely removing the gallbladder.
Compared with open surgery (which requires a larger incision), laparoscopic surgery usually results in:
- Smaller scars and better cosmetic outcomes
- Shorter hospital stays (often going home the next day)
- Faster recovery with less pain
- Lower risk of complications such as infection and bleeding
Types of Laparoscopic Cholecystectomy Procedure
The choice of surgical approach depends on the patient's overall health, the severity of gallbladder disease, and the surgeon's expertise. Common approaches include:
Conventional Laparoscopic Cholecystectomy
- Involves four small incisions in the abdomen.
- Instruments are inserted through these incisions to remove the gallbladder.
- Considered the standard method and is the most widely performed technique.
Single-Incision Laparoscopic Cholecystectomy (SILC)
- Performed through one incision near the belly button.
- Leaves a nearly scarless appearance, making it a preferred option for patients concerned about cosmetics.
- May take longer and is technically more complex, so it is not suitable for all patients.
Laparoscopic Cholecystectomy with Intraoperative Cholangiography (IOC)
- Involves injecting a special dye into the bile ducts during surgery.
- Real-time X-ray images help the surgeon check for stones in the bile duct and ensure that the anatomy is clear before removal.
- Recommended in patients with a history of jaundice, pancreatitis, or suspected bile duct stones.
1-2 Hours
Surgery Duration
General Anesthesia
Anesthesia Used
4-6 Weeks
Full Recovery Timeline

When is Laparoscopic Cholecystectomy Recommended?
Laparoscopic cholecystectomy is most often performed when the gallbladder is causing health problems that cannot be managed with lifestyle changes or medication. Doctors recommend this minimally invasive procedure in the following situations:
Gallstones Causing Symptoms
- Biliary colic (gallbladder pain): Sharp or cramping pain in the upper right abdomen, often after fatty meals.
- Digestive issues: Recurrent bloating, nausea, or indigestion linked to gallstones.
- Impact on quality of life: When pain episodes become frequent or severe enough to limit daily activities.
Inflammation of the Gallbladder (Cholecystitis)
- Acute cholecystitis: A sudden infection and swelling of the gallbladder, usually caused by a blocked bile duct.
- Chronic cholecystitis: Long-standing irritation from gallstones leading to thickened gallbladder walls and recurring discomfort.
Gallstones in the Bile Ducts (Choledocholithiasis)
- Obstructed bile flow: Stones may travel from the gallbladder into the common bile duct, causing jaundice (yellowing of the skin and eyes).
- Pancreatitis risk: Blocked bile ducts can trigger inflammation of the pancreas, a painful and potentially serious condition.
Gallbladder Polyps
- Size matters: Polyps larger than 1 cm are considered risky because of their potential to develop into cancer.
- Precautionary removal: Even smaller polyps may be removed if they grow over time or occur alongside gallstones.
How to Prepare for Laparoscopic Cholecystectomy?
Preparing well for laparoscopic cholecystectomy makes surgery safer and recovery smoother. Simple steps before the procedure can lower risks and improve healing.
Why preparation matters:
- Lowers risk of bleeding and infection.
- Helps the team plan anesthesia.
- Makes your first days at home easier.
Medical evaluation and tests
- History and exam: Share past illnesses, allergies, and prior surgeries.
- Medicine review: Bring a list of every pill and supplement you take.
- Tests: You may need blood tests, an ultrasound, and an ECG.
- Anesthesia check: Tell them about loose teeth, sleep apnea, or reflux.
- Consent: Ask about benefits, risks, and other options.
Medicine plan (very important)
Do not change pills on your own. Your surgeon or anesthetist will guide you.
- Blood thinners: You may need to pause these before surgery.
- Pain pills: Avoid ibuprofen and similar NSAIDs unless your doctor says OK.
- Diabetes pills/insulin: Doses may change around the fasting period.
- Blood pressure pills: Most are continued; some may be held the morning of surgery.
- Herbal products and vitamins: Many increase bleeding. You may be told to stop them.
- Bring inhalers, eye drops, and CPAP (if used).
Lifestyle steps that help healing
- Stop smoking: Quitting even 2-4 weeks before helps your lungs heal.
- No alcohol: Avoid alcohol for at least 48-72 hours before surgery.
- Move daily: Gentle walks improve lung function and mood.
- Sleep well: Aim for 7-8 hours the week before surgery.
Nutrition and hydration
- Simple, low-fat meals: Less strain on your gallbladder before surgery.
- Hydrate well: Drink water through the day until your fasting time starts.
- Bowel routine: A laxative is rarely needed. Ask if you tend to be constipated.
- Supplements: Do not start new ones this week unless advised.
Infection and skin prep
- Skin wash: Use plain soap or the cleanser your hospital gives.
- Do not shave: Shaving raises infection risk. The team will clip if needed.
- Mouth and teeth: Brush and floss the night before.
- Feeling unwell: Fever, cough, or rash, call our team before you come in.
Home preparation
- Support person: Arrange help for the first 24-48 hours.
- Food: Prepare light, low-fat meals and clear soups.
- Essentials within reach: Meds, water, charger, pillows, and a small trash bin.
- Safe space: Clear walkways. Set up a chair with arms for easy standing.
- Transport: You must not drive after anesthesia. Plan your ride home.
The day before surgery
- Fasting rules: Solid food stops after midnight. Clear liquids are sometimes allowed until 2 hours before arrival.
- Shower: Use the advised cleanser. Dry with a clean towel.
- Medications: Take only those you were told to take.
- No makeup, lotions, or nail polish: They can affect monitors and cleaning.
- Bag ready: Pack ID, reports, med list, glasses, and CPAP if used.
- Sleep: Aim for a calm evening and an early night.
The morning of surgery
- No food or drink unless told otherwise.
- Take approved meds with small sips of water.
- Wear loose clothes and slip-on shoes.
- Leave valuables at home.
- Arrive early: Check in, sign forms, and meet your care team.
- Marking and checks: The team confirms your name, procedure, and side.
- Anesthesia talk: Ask about nausea control and pain relief plans.
If surgery may be delayed
Call your surgeon before you leave home if you have:
- Fever, chest pain, a bad cough, or trouble breathing.
- A positive test for flu, COVID-19, or strep.
- A new wound, rash, or urinary symptoms.
What Happens During Laparoscopic Cholecystectomy?
Laparoscopic cholecystectomy steps are performed in a structured way to ensure safety. The procedure usually takes 1-2 hours and is done under general anesthesia to ensure the patient feels no pain.
Preparation & Anesthesia
- Before surgery, the patient changes into a hospital gown and an intravenous (IV) line is placed to give fluids and medications.
- General anesthesia is administered, which means the patient will be completely asleep and pain-free during the operation.
- Once anesthesia takes effect, a breathing tube may be inserted to support breathing.
Incision & Access Point
- The surgeon makes 3-4 small cuts in the abdomen, usually less than 1 cm each.
- Through these incisions, a laparoscope (a thin tube with a tiny camera) and special surgical instruments are inserted.
- Carbon dioxide gas is gently introduced into the abdomen to inflate it slightly, giving the surgeon more space to see and work safely.
Removal of the Gallbladder
- The surgeon uses the laparoscope to clearly view the gallbladder and surrounding structures on a monitor.
- The cystic duct (which carries bile) and the cystic artery (which supplies blood) are carefully identified, clipped, and cut.
- The gallbladder is then gently separated from the liver bed using precise instruments.
- Finally, the gallbladder is removed through one of the small incisions.
Closure of Incisions
- After removal, the carbon dioxide gas is released from the abdomen.
- The small incisions are then closed using dissolvable stitches, surgical glue, or tiny adhesive strips.
- In many cases, no large external dressing is needed, leaving minimal scars.
Recovery Room Observation
- Once the surgery is complete, the patient is moved to a recovery room.
- Nurses monitor vital signs, such as heart rate, blood pressure, and oxygen levels, until the effects of anesthesia wear off.
- Pain relief medication and anti-nausea drugs may be given if needed.
- Most patients can return home the same day, though some may stay overnight for observation.
Who Will Perform the Laparoscopic Cholecystectomy?
Laparoscopic cholecystectomy is a surgical procedure performed by surgeons, who are specialized medical professionals. These surgeons have expertise in minimally invasive surgical techniques and are trained to operate using laparoscopic instruments and technology.
Here are the types of specialists who commonly perform laparoscopic cholecystectomy:
What to Expect After Laparoscopic Cholecystectomy Surgery?
Recovery after a laparoscopic cholecystectomy is usually smooth and much faster than open gallbladder surgery. Most patients heal well with proper rest, pain management, and gradual return to activities.
First Few Days After Surgery
- Pain and Discomfort: Mild pain, bloating, or shoulder ache is common due to the gas used during surgery. Painkillers usually provide relief.
- Movement: Gentle walking is encouraged as soon as possible. It improves blood flow, reduces the risk of clots, and helps ease bloating.
- Diet: Patients start with light meals. Fatty or spicy foods may cause discomfort at first.
Weeks 2-4
- Healing Progress: Most patients return to desk jobs or light household work during this period.
- Wound Care: Small scars begin to fade. Keeping the area clean and dry prevents infection.
- Energy Levels: Fatigue is normal but improves with rest and a balanced diet.
Weeks 5-6
- Activity Level: Patients can resume almost all normal activities, including mild exercise.
- Restrictions: Avoid heavy lifting or strenuous workouts until your surgeon approves.
- Digestive Adjustment: Some people notice changes in bowel habits, which usually settle over time.
3-6 Months
- Full Recovery: By this stage, most patients feel completely recovered.
- Scars: Laparoscopic scars are very small and often fade to become barely visible.
- Long-Term Outlook: The body adapts well to life without a gallbladder, and patients usually return to a normal diet.
Benefits of Laparoscopic Cholecystectomy
Laparoscopic cholecystectomy, often called keyhole gallbladder surgery, is considered the gold standard treatment for gallstones and certain gallbladder diseases. Compared to the traditional open surgery, it offers several important benefits:
- Smaller scars and better cosmetic outcome: Since the surgery is performed through 3-4 very small incisions, scarring is minimal and often hardly visible after healing. This makes it cosmetically more appealing, especially for younger patients.
- Shorter hospital stay: Most patients go home within 24-48 hours. In many cases, it can even be done as a day-care procedure, meaning patients are discharged the same day.
- Faster recovery and return to daily life: People can usually resume light activities within a week and return to work or school in about 10-14 days, much faster than with open surgery.
- Less pain after surgery: The smaller incisions mean patients usually need less pain medication and experience a more comfortable recovery.
- Lower risk of complications: Laparoscopic techniques reduce the risk of wound-related problems, such as infection or hernia, compared to open surgery.
Risks of Laparoscopic Cholecystectomy
Like any surgery, laparoscopic cholecystectomy carries certain risks. Fortunately, these complications are uncommon and most patients recover without issues. Possible risks include:
- Bleeding or infection: Although rare, bleeding from blood vessels or infection at the incision site can occur. These are usually managed with medication or, in rare cases, further treatment.
- Bile duct injury: Damage to the bile ducts is one of the most serious but rare complications. If it occurs, additional surgery or procedures may be needed to repair it.
- Risks related to anesthesia: As with any surgery under general anesthesia, there is a very small risk of breathing problems, allergic reactions, or heart-related complications.
- Hernia at the incision site: In some patients, a small bulge (hernia) may develop where the instruments were inserted. This is uncommon and can be corrected if necessary.
Cost of Laparoscopic Cholecystectomy in India
The cost of a laparoscopic cholecystectomy in India can vary depending on factors such as the complexity of your case, the surgeon's experience, and the type of hospital facilities chosen. On average, the surgery may range between Rs. 45,000 and Rs. 1,00,000.
Every patient's treatment journey is unique, so the exact cost can only be confirmed after a medical evaluation.
To get a personalised estimate and understand what's included in the package, please contact our support team today.