What Is a Pulmonary Valve Surgery?
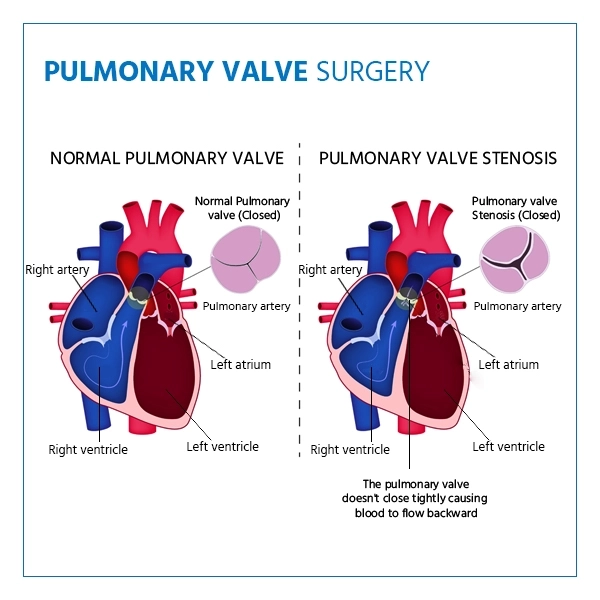
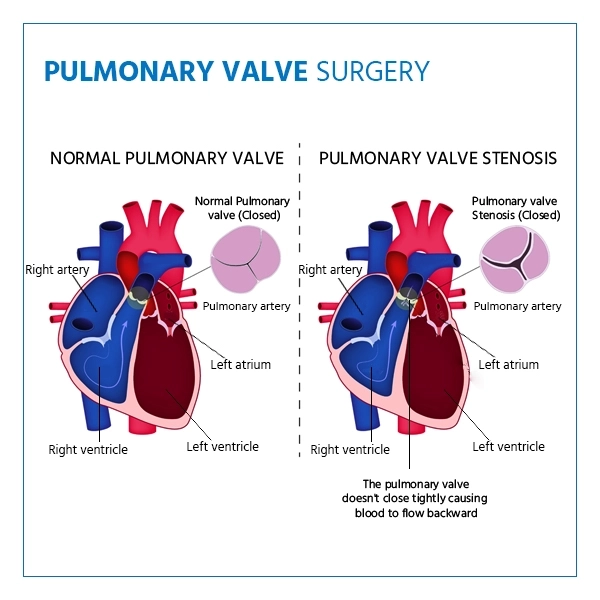
Pulmonary valve surgery is a heart procedure performed to repair or replace the pulmonary valve, which controls blood flow from the right ventricle of the heart to the lungs. When the valve becomes narrowed (stenosis) or leaky (regurgitation), it can disrupt normal circulation and strain the heart.
This surgery helps restore proper blood flow and improve overall heart function. It is often recommended for patients with congenital heart defects, valve damage from infection, or severe valve dysfunction that medications and other treatments cannot correct.
It's important to understand that pulmonary valve surgery is not a preventive measure but a corrective treatment for significant valve problems that affect heart health.
Types of Pulmonary Valve Surgery
According to trusted medical resources, there are several types of Pulmonary Valve Surgery.
- Pulmonary Valve Stenosis: This is a valve narrowed by a heart defect that does not allow the heart to pump out blood to the lungs. Surgery is recommended in case of progression of symptoms like fatigue or shortness of breath.
- Pulmonary Valve Regurgitation: A damaged valve can make the blood go backwards and put pressure on the heart, which results in symptoms such as breathlessness and a lack of exercise capacity.
- Tetralogy of Fallot (TOF): A complicated congenital heart disease which involves defects of the pulmonary valves and other structural cardiac problems. Corrective surgery is performed on many patients during childhood, and later during adulthood, valve replacement can be necessary as the pulmonary valve can be defective or leaky later in life.
- Dysfunctional Bioprosthetic Valve: Patients who have already had a biological (tissue) valve replacement may eventually experience valve deterioration. A worn-out valve can cause either narrowing or leakage, requiring another surgery or transcatheter replacement to restore proper heart function.
- Conduit Dysfunction: Sometimes, a conduit (a surgically placed tube that connects the right ventricle to the pulmonary artery) is used in patients with congenital heart defects. Over time, these conduits can narrow or leak, and surgery may be needed to repair or replace them.
- Endocarditis: This is a serious infection that damages the pulmonary valve tissue. If the infection leads to valve destruction or dysfunction, surgery becomes essential to remove the infected tissue and replace the valve.
- Right Ventricular Outflow Obstruction: A blockage in the pathway carrying blood from the right ventricle to the pulmonary artery can occur due to congenital defects or scar tissue from previous surgeries. Surgery is performed to remove the obstruction and restore smooth blood flow.
3-5 Hours
Surgery Duration
General Anesthesia
Anesthesia Used
6 to 12 weeks
Full Recovery

When is Pulmonary Valve Surgery Recommended?
Pulmonary valve surgery is usually advised when valve problems begin to affect heart function or cause troubling symptoms. Based on clinical guidelines, here are the main situations where doctors may recommend it:
- Severe Pulmonary Valve Stenosis: When the valve is too narrow and restricts blood flow to the lungs, leading to chest pain, fainting, or breathlessness. Surgery helps relieve the obstruction and restore normal circulation.
- Pulmonary Valve Regurgitation: If the valve is leaky and allows blood to flow backward into the heart, it can cause the heart to enlarge and weaken over time. Surgery is needed when symptoms such as fatigue or swelling appear.
- Congenital Heart Conditions (like Tetralogy of Fallot): Children and adults with congenital defects involving the pulmonary valve often require surgery to correct valve function and prevent long-term complications.
- Failed Previous Valve Surgery (Bioprosthetic Valve Dysfunction): If a tissue valve replacement wears out or stops working properly, a repeat surgery or catheter-based replacement may be necessary.
- Conduit Dysfunction or Outflow Tract Obstruction: Patients with a surgically placed conduit or narrowing in the right ventricular outflow tract may need surgery to maintain healthy blood flow to the lungs.
- Infective Endocarditis: If the pulmonary valve is severely damaged due to infection, surgical replacement may be the safest option.
Preparing for Pulmonary Valve Surgery Procedure
Preparing for your Pulmonary Valve Surgery is a key part for a smooth surgery and a fast recovery.
Medical Evaluation & Pre-Op Tests
- Share your complete medical history, including heart conditions, medications, and allergies.
- Your doctor may order tests such as blood work, chest X-ray, echocardiogram, ECG, or cardiac catheterization to assess your heart function.
- Ensure all test results are completed and reviewed well before the surgery date so your care team can finalize the plan.
Health Habits & Lifestyle Adjustments
- Quit smoking at least 4-6 weeks before surgery as it reduces oxygen supply and slows healing.
- Avoid alcohol and blood-thinning medications (aspirin, NSAIDs, vitamin E, and certain herbal supplements) at least 1-2 weeks before surgery, unless cleared by your doctor.
- Follow a heart-healthy diet with plenty of protein, vitamins, and minerals to prepare your body for recovery.
- Stay physically active as advised, but avoid overexertion.
Preparing Your Home and Support System
- Arrange for a family member or friend to take you to the hospital and be available to help during the first days of recovery.
- Prepare your living space with easy-to-reach essentials like water, prescribed medications, loose clothing, and extra pillows for comfort.
- Plan your meals ahead of time, focusing on light and nutritious options to aid recovery.
The Day Before & Day of Surgery
- Follow your doctor's fasting instructions, usually no food or drink after midnight before surgery.
- Take only the medications approved by your surgeon on the morning of surgery with a small sip of water.
- Bathe as instructed, using antiseptic soap if recommended. Avoid using lotions, deodorants, perfumes, nail polish, or jewelry.
- Wear comfortable, front-opening clothes to the hospital for convenience after surgery.
What Happens During Pulmonary Valve Surgery?
During surgery, the pulmonary valve is either repaired or replaced, sometimes using open-heart techniques or minimally invasive approaches, depending on the patient's condition.
Preparation & Anesthesia
On the day of surgery, you'll meet your cardiac surgical team to review the procedure and address any last-minute questions. Once in the operating room, general anesthesia is administered, ensuring you are completely asleep and comfortable throughout the surgery.
Accessing the Heart
Depending on the type of surgery, the surgeon may perform open-heart surgery through a midline chest incision or use a minimally invasive approach with smaller incisions. For catheter-based procedures (like TPVR), access is through a vein, usually in the groin.
Valve Repair or Replacement
- Valve Repair: The surgeon reshapes, widens, or patches the existing pulmonary valve to restore proper function.
- Valve Replacement: The damaged valve is removed and replaced with either a mechanical valve (durable, requires blood-thinning medications) or a biological valve (tissue valve, may require replacement in the future).
Restoring Blood Flow
Once the valve is repaired or replaced, the heart is carefully tested to ensure blood flows smoothly from the right ventricle to the lungs. Any supporting conduits or surrounding tissues may also be adjusted if needed.
Closing the Incisions
The chest is closed with sutures or staples, and the area is dressed with sterile bandages. For open-heart procedures, temporary drains may be placed to remove excess fluid.
Immediate Recovery
You will be moved to the ICU for close monitoring. Patients are usually encouraged to start light movements within a day to promote circulation and reduce complications. Pain management, breathing exercises, and gentle mobility are key parts of the early recovery period.
Recovery After Pulmonary Valve Surgery Procedure
Recovering from a Pulmonary Valve Surgery is a step-by-step process, and real care makes all the difference.
Hospital Stay
- Open-heart surgery patients typically stay 5-7 days in the hospital, including a few days in the ICU for close monitoring.
- Minimally invasive or transcatheter procedures may have a shorter stay, often 2-4 days.
Immediate Post-Operative Care
- Heart rate, blood pressure, oxygen levels, and incision sites are closely monitored.
- Pain management is provided to keep you comfortable while encouraging movement and breathing exercises.
- Small drains or tubes may be temporarily placed to remove excess fluid or blood.
At-Home Recovery
- Most patients gradually resume normal daily activities over 6-12 weeks.
- Avoid heavy lifting, strenuous exercise, or activities that strain the chest until cleared by your doctor.
- Follow prescribed medications, including blood thinners if you received a mechanical valve.
- Eat a heart-healthy diet and maintain hydration to support healing.
Follow-Up & Rehabilitation
- Regular follow-up visits are scheduled to monitor heart function and valve performance.
- Cardiac rehabilitation programs may be recommended to improve stamina, strengthen the heart, and ensure safe recovery.
Lifestyle Changes After Pulmonary Valve Surgery
- Maintain a balanced diet, exercise moderately as advised, and avoid smoking or excessive alcohol.
- Watch for symptoms like swelling, breathlessness, fever, or unusual pain, and report them promptly to your doctor.
Recovery is gradual, but with proper care and adherence to medical advice, most patients experience improved heart function, better energy levels, and an enhanced quality of life.
Benefits of Pulmonary Valve Surgery
The surgery improves blood flow, relieves symptoms, enhances heart function, and prevents complications related to valve disease.
- Improved Heart Function: Regains normal blood flow in the heart to lungs and the heart works less.
- Relief from Symptoms: Minimizes symptoms of breathlessness, fatigue, swelling and chest pains that are a result of valve dysfunction.
- Prevention of Complications: Helps prevent heart enlargement, arrhythmias, and heart failure that can result from untreated valve problems.
- Enhanced Quality of Life: Increases energy, exercise tolerance, and overall well-being.
- Long-Term Heart Health: Correcting the valve problem improves survival rates and decreases future cardiac
Risks of Pulmonary Valve Surgery
Potential risks include infection, bleeding, arrhythmias, valve malfunction, or complications from anesthesia.
- Bleeding or Infection: As with any surgery, there is a risk of bleeding at the incision site or infection.
- Blood Clots: Formation of clots can occur, which may require medication or intervention.
- Arrhythmias: Irregular heartbeats can develop temporarily or rarely persist long-term.
- Valve Dysfunction: In some cases, the repaired or replaced valve may not work perfectly or may wear out over time.
- Stroke or Heart Attack: Rare but serious complications may occur during or after surgery.
- Other Surgical Risks: Reactions to anesthesia, lung complications, or other organ issues can happen depending on overall health.
Cost of Pulmonary Valve Surgery in India
The cost of pulmonary valve surgery depends on the type of procedure (open-heart, minimally invasive, or transcatheter), the choice of valve (mechanical or biological), length of hospital stay, and the surgeon's experience. On average, pulmonary valve surgery can range from Rs. 1,50,000 to Rs. 5,00,000, depending on complexity and valve type.