What is a Myomectomy Surgery?
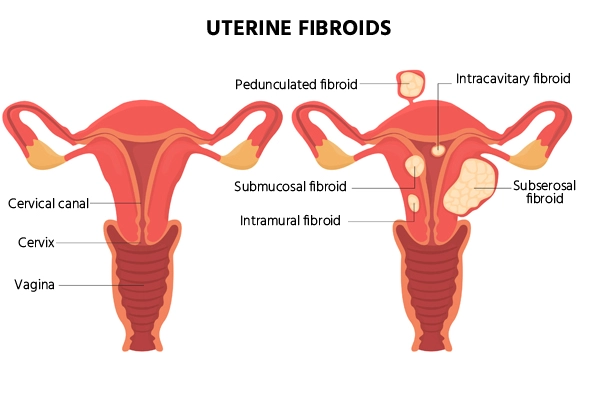
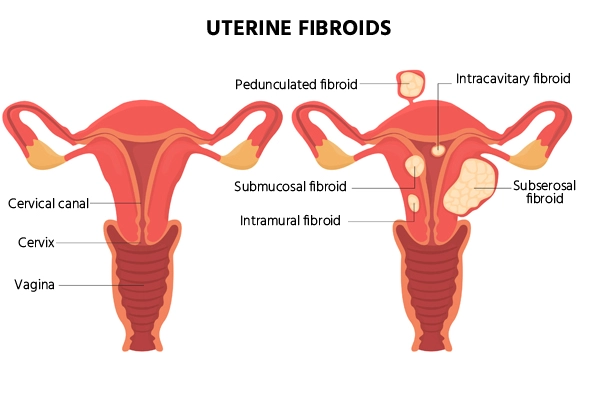
Myomectomy is a surgical procedure used to remove fibroids from the uterus. Uterine Fibroids are non-cancerous growths that can develop in or around the uterus and cause symptoms like heavy bleeding, pelvic pain, and pressure. This surgery aims to preserve the uterus, making it an option for women who wish to maintain their fertility.
Unlike a hysterectomy, which involves the complete removal of the uterus, myomectomy focuses on the targeted removal of fibroids while preserving the uterus.
This makes myomectomy an ideal choice for women who want to retain their uterus and experience fewer body changes after myomectomy compared to uterus removal.
Types of Myomectomy
- Abdominal Myomectomy: This is the most common approach, where a larger incision is made in the abdomen to remove the fibroids. It's typically used when fibroids are large or located deep within the uterus.
- Laparoscopic Myomectomy (Minimally Invasive): This procedure uses small incisions and a camera (laparoscope) to guide the surgeon in removing the fibroids. It's a less invasive option, leading to quicker recovery times and less scarring.
- Hysteroscopic Myomectomy: Used for fibroids inside the uterus (submucosal fibroids), this procedure is performed through the cervix using a scope. It doesn't require any incisions on the abdomen, making it the least invasive option.
- Robotic-Assisted Myomectomy: A more advanced form of laparoscopic surgery, robotic-assisted myomectomy uses robotic arms controlled by the surgeon for greater precision in removing the fibroids. It combines the benefits of minimally invasive surgery with enhanced accuracy.
1-3 Hours
Surgery Duration
General Anesthesia
Anesthesia Used
2-6 Weeks
Full Recovery Timeline

Indications of Myomectomy Surgery Procedure
Myomectomy surgery procedure is indicated for various medical conditions and situations where uterine fibroids are causing significant symptoms or affecting a woman's reproductive health.
Some of the common indications for myomectomy include:
- Symptomatic Uterine Fibroids: When fibroids cause symptoms such as heavy menstrual bleeding(menorrhagia), prolonged menstrual periods, pelvic pain, lower back pain, and pressure on the bladder or rectum, myomectomy can provide relief by removing the source of these symptoms.
- Infertility: Women experiencing difficulty conceiving due to fibroids may opt for myomectomy to improve their chances of pregnancy. Fibroids can sometimes interfere with the implantation of a fertilised egg or lead to miscarriages.
- Desire to Preserve Uterus: Myomectomy is chosen by women who want to retain their uterus for future reproductive or personal reasons as an alternative to a hysterectomy, which involves the complete removal of the uterus.
- Large Fibroids: When fibroids are particularly large, causing discomfort or complications, myomectomy may be recommended to alleviate symptoms and prevent potential complications.
- Abnormal Bleeding: Fibroids can lead to heavy, prolonged menstrual periods (menorrhagia), and myomectomy helps reduce or eliminate excessive bleeding.
- Pelvic Pain: When fibroids cause chronic or severe pelvic pain, a myomectomy may be performed to alleviate the discomfort.
- Pressure on Surrounding Organs: Large fibroids pressing on the bladder or rectum can cause urinary issues or constipation, and myomectomy may be recommended to relieve these symptoms.
- Prolapsed Fibroids: If fibroids protrude into the vaginal canal, they can cause discomfort and require removal through myomectomy.
- Desire to Preserve Fertility: Myomectomy is suitable for women who wish to preserve their uterus and fertility, as it removes fibroids while keeping the uterus intact, thus helping to avoid extensive body changes after uterus removal.
When Would a Doctor Recommend Myomectomy?
- When fibroids are causing significant symptoms affecting the quality of life
- If fibroids interfere with fertility or pregnancy
- For women who wish to preserve their uterus and avoid a hysterectomy
- When fibroids are large, growing rapidly, or causing organ pressure.
How to Prepare for Myomectomy Surgery?
Preparing for myomectomy surgery involves several steps to ensure a smooth procedure and a successful recovery.
Here's a general guideline on how to prepare for myomectomy surgery:
- Consultation and Evaluation: Schedule a consultation with your gynecologist or the surgeon who will perform the myomectomy. Discuss your medical history, current medications, allergies, and any pre-existing conditions.
- Preoperative Instructions: Your surgeon will provide specific preoperative instructions, which may include guidelines on eating and drinking before the surgery and any necessary fasting.
- Smoking and Alcohol: If you smoke, consider quitting or at least reducing smoking before the surgery, as smoking can impair healing and increase the risk of complications.
- Nutrition and Hydration: Focus on a balanced diet rich in nutrients to support your body's healing process.
- Arrange Support: Depending on the type of myomectomy and the expected recovery time, you might need assistance with daily activities during the initial recovery period. Arrange for someone to help you if needed.
- Mental and Emotional Preparation: Understand the procedure, potential risks, and expected outcomes. Discuss any concerns or questions with your surgeon.
- Arrangements for Transportation: Arrange for transportation to and from the hospital on the day of the surgery, as you may not be able to drive yourself after the procedure.
What Happens During a Myomectomy Surgery?
During a myomectomy, your surgeon carefully removes fibroids from the uterus while keeping the uterus intact. The exact steps may vary depending on the size, number, and location of the fibroids.
- Abdominal Myomectomy (Open Surgery): In this traditional procedure, the surgeon makes an open incision in the abdomen to access and remove the fibroids. This method is often used for larger or multiple fibroids that are difficult to remove using minimally invasive techniques.
- Laparoscopic Myomectomy: This minimally invasive approach involves small incisions and the use of a laparoscope (a camera) to guide the removal of fibroids. The procedure is less invasive, resulting in less scarring and a quicker recovery compared to open Laparoscopic surgery.
- Robotic-Assisted Myomectomy: A robotic system helps guide the surgeon's precise movements. It enhances dexterity and visualization, allowing for a more accurate removal of fibroids, particularly in challenging areas.
- Hysteroscopic Myomectomy: This technique is used when fibroids are within the uterine cavity or protruding into it. A hysteroscope is inserted through the cervix, enabling the surgeon to remove fibroids without making external incisions.
Who will Perform Myomectomy Surgery?
Here are the types of specialists who may be involved in treating myomectomy surgery:
- Gynecologist
- Gynecologic Surgeon
- Reproductive Endocrinologist
- Minimally Invasive Surgeon
- Urogynecologist
- Hysteroscopic Surgeon
Recovery After Myomectomy Surgery Procedure
Recovery after a myomectomy surgery procedure can vary based on the type of surgery performed (open, laparoscopic, robotic, hysteroscopic), the size and number of fibroids removed, and individual factors such as overall health and age.
Here's a general overview of what you might expect during the recovery period:
- Hospital Stay: After the surgery, you will be monitored in the recovery area until you are awake and stable.
- First Few Days After Surgery: Pain and discomfort are common in the first few days. Your healthcare team will provide pain medication and instructions on how to manage pain.
- First Two Weeks: You may need to take time off work or limit physical activities during this period to aid healing. During this time, some patients notice mild body changes after myomectomy, such as hormonal fluctuations or slight weight changes, which are usually temporary.
- 2-6 Weeks: Pain and discomfort usually improve during this time, although some residual soreness might persist.
- Long-Term Recovery: Over the next few months, your energy levels should return to normal, and any residual discomfort should gradually diminish.
Lifestyle Changes After Myomectomy Surgery Procedure
After undergoing a myomectomy surgery procedure, making certain lifestyle changes can aid in your recovery and overall well-being.
Here are some recommended lifestyle adjustments to consider:
- Diet and Nutrition: Focus on a balanced diet rich in fruits, vegetables, lean proteins, and whole grains to support healing and boost your immune system. Stay hydrated by drinking plenty of water.
- Physical Activity: Follow your surgeon's guidelines on physical activity and exercise. Start with gentle walking and gradually increase your activity level as you heal.
- Rest and Sleep: Get adequate rest to allow your body to heal properly. Prioritize sleep and consider adjusting your sleep position to avoid putting pressure on your surgical site.
- Medications: Take any prescribed medications as directed by your healthcare provider. If you're on pain medication, follow the recommended dosages and consult your doctor if you have concerns about side effects.
- Stress Management: Practice relaxation techniques, meditation, or deep breathing exercises to manage stress and promote healing.
- Clothing and Comfort: Wear loose and comfortable clothing to avoid putting pressure on the surgical area.
- Alcohol and Smoking: If you smoke, consider quitting or reducing smoking, as it can hinder the healing process.
- Work and Activities: Discuss with your surgeon when it's safe to return to work and resume normal activities.
Benefits of Myomectomy Surgery
- Symptom Relief: Reduces heavy menstrual bleeding (menorrhagia), prolonged periods, and pelvic pain. Alleviates pressure on the bladder and bowel caused by fibroids, improving overall comfort.
- Fertility Preservation: Removes fibroids while preserving the uterus, enhancing the chances of conception. Reduces the risk of miscarriage or infertility caused by fibroid interference with embryo implantation.
- Uterus Preservation: Unlike hysterectomy, myomectomy keeps the uterus intact, allowing for future pregnancies and maintaining hormonal function.
- Improved Quality of Life: Reduces discomfort, pelvic pressure, and urinary or bowel symptoms, leading to improved daily functioning and overall well-being.
- Targeted Treatment Approach: Specifically removes fibroids while preserving healthy uterine tissue. Offers minimally invasive options (laparoscopic, hysteroscopic, or robotic-assisted) that result in smaller scars, shorter hospital stay, and quicker recovery.
Complications of Myomectomy
- Infection: Any surgical procedure carries a risk of infection at the incision sites.
- Excessive Bleeding: In some cases, fibroids can be large, and removing them may cause bleeding.
- Damage to Surrounding Organs: In rare cases, adjacent organs such as the bowel may be injured.
- Recurrent Fibroids: Fibroids may return after the surgery, especially if only a portion of the fibroids was removed.
How much does a Myomectomy Cost in India?
The cost of myomectomy surgery in India generally ranges from Rs. 40,000 to Rs. 2,75,000 or more, depending on the type of procedure, hospital, surgeon's expertise, and complexity of the case. Hysteroscopic myomectomy is usually the least expensive, while robotic procedures are the most costly.
Factors Influencing Myomectomy Cost:
- Surgical Approach: Abdominal, hysteroscopic, laparoscopic, or robotic methods significantly affect cost.
- Hospital Choice: Premium hospitals typically charge more than standard facilities.
- Surgeon's Expertise: Experienced or renowned surgeons often have higher fees.
- Complexity of Fibroids: Number, size, location, and severity of fibroids influence surgical difficulty and cost.
- Geographical Location: Costs vary depending on the city or region within India.