What is Pleural Effusion?
A pleural effusion is a collection of fluid around the lungs that is unusually large. Because it can be caused by a variety of medical disorders, even if the pleural effusion needs to be drained, the doctor will most likely address the underlying cause. The pleura is a thin membrane that borders the interior of the chest wall and the surface of the lungs. Fluid builds up between the layers of the pleura when you have a pleural effusion. Usually, a few teaspoons of watery fluid are normally present in the pleural space, allowing your lungs to move freely in your chest cavity while you breathe.
Pleural Effusion Symptoms
Some people with this condition have no symptoms and are diagnosed after a chest x-ray is taken for another cause. The ailment or condition that created the effusion may lead the patient to have unrelated symptoms. Pleural effusion symptoms include
- Chest discomfort is generally a sharp aching that is amplified by coughing or taking heavy breaths.
- Fever and chills with a cough
- Hiccups
- Breathing quickly
- Breathing problems
- There are times when there are no symptoms.
Pleural Effusion Causes
It can be caused by a variety of factors. The following are a few of the more common ones:
- Leaking from other organs: This commonly happens if you have congestive heart failure, which occurs when the heart fails to adequately pump blood to your body. It can also be caused by fluid buildup in the body, which seeps into the pleural space, as a result of liver or renal dysfunction.
- Cancer: Lung cancer is the most common cause, although other malignancies that have progressed to the lung or pleura can also cause it.
- Infections: Pneumonia and TB are two disorders that can cause pleural effusion.
- Autoimmune conditions: Lupus or rheumatoid arthritis are some diseases that can cause it.
- Pulmonary embolism: Pleural effusion might result from a blockage in an artery in one of the lungs.
Risks factors of Pleural Effusion
The following are some of the most common risk factors:
- Chronic smokers
- Alcohol abuse
- Neoplasia (e.g. lung cancer patients)
- Liver cirrhosis
- Use of certain medications (e.g. dasatinib in the treatment of patients with chronic myelogenous leukaemia and immunosuppressive medicine)
- Existing pulmonary illness or injury
- Occupational exposure to asbestos
- Heart failure
Surgery-related risk factors include the following:
- Lower preoperative oxygen saturation
- Smaller conduit size
- Longer duration of cardiopulmonary bypass
- Presence of postoperative infection
Complications of Pleural Effusion
The following are some of the possible side effects:
- Lung scarring,
- Pneumothorax (collapse of the lung) as a complication of thoracentesis,
- Empyema (a collection of pus within the pleural space), and
- Sepsis (blood infection) sometimes can be fatal
Diagnosis
The doctor will do a physical examination and perform imaging tests, such as a CT scan to establish you have a pleural effusion. The commonly recommended tests include:
- Chest X-ray: On X-rays, pleural effusions show white, whereas air space appears black. If a pleural effusion is suspected, further X-ray films may be taken while you lie on your side. These can demonstrate if the fluid in the pleural space is flowing smoothly.
- Computed tomography (CT scan): A CT scanner swiftly collects a large number of X-rays, and a computer creates pictures of the entire chest; inside and out. CT scans provide more information than chest X-rays.
- Blood tests: A blood test might reveal whether or not you have an infection. Other blood tests may be used to diagnose autoimmune diseases like rheumatoid arthritis or lupus. Pleurisy might be the initial indication of many illnesses.
- Ultrasound: Pictures of the inside of the body are generated by a probe on the chest and shown on a video screen. The doctor may use ultrasound to find the fluid so that a sample may be taken for testing.
- Electrocardiogram (ECG or EKG): This heart-monitoring test may be suggested to rule out certain cardiac disorders as a possible cause of chest discomfort. The doctor may also perform a technique known as thoracentesis. They'll test a small amount of the fluid. They accomplish this by inserting a needle and a catheter into the pleural area between your ribs.
Pleural Effusion Treatment
The underlying illness and whether the effusion is producing significant respiratory symptoms, such as shortness of breath or trouble breathing, determine the treatment for pleural effusion.
Procedures for pleural effusion treatment include:
- Thoracentesis: If the effusion is big, the doctor may remove more fluid for testing than is necessary solely to relieve the discomfort.
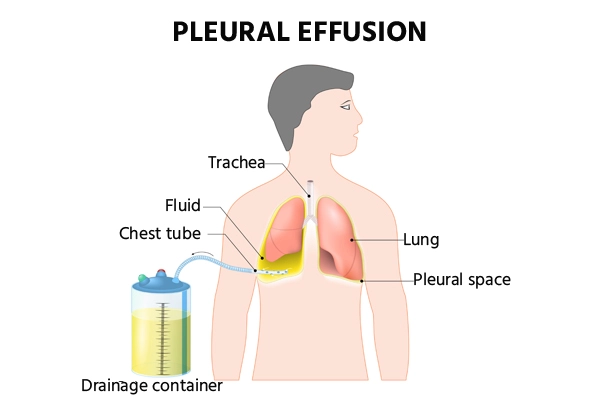
- Tube thoracostomy (chest tube): Your doctor makes a small cut in your chest wall and puts a plastic tube into your pleural space for several days.
- Pleural drain: If the pleural effusions recur, the doctor may insert a long-term catheter into the pleural space via the skin. It can then be drained at home. The doctor will instruct patients on how to proceed and when to do so.
- Pleurodesis: Through a chest tube, the doctor injects talc or doxycycline into the pleural space. The chemical causes the pleura and chest wall to become inflamed, causing them to bond closer together as they recover. Pleurodesis can often prevent pleural effusions from returning.
- Pleural decortication: Inside the pleural space, surgeons can eliminate potentially hazardous inflammation and bad tissue. To do so, the surgeon may make tiny or large incisions (thoracoscopy) or (thoracotomy).
