What is Bronchiectasis?
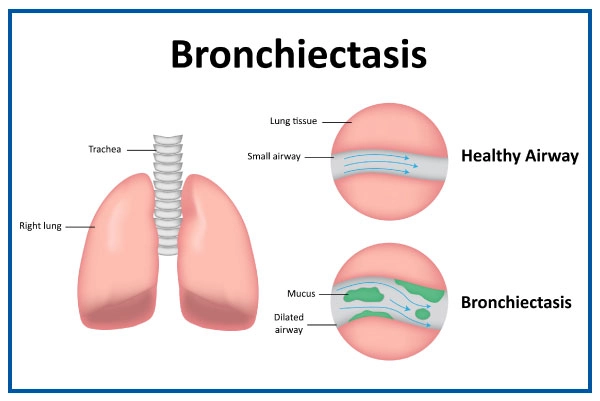
Bronchiectasis is a respiratory disease in which the bronchial tubes get permanently damaged, swollen, and thickened. Germs and mucus build up in the lungs due to clogged airways, thus increasing the risk of respiratory infection and airway blockages. Bronchiectasis is a chronic condition that worsens over time.
- Bronchiectasis is a pulmonary disease that currently lacks a cure, but it can be effectively treated.
- By undergoing treatment, individuals with bronchiectasis can maintain a normal lifestyle.
- It is crucial to promptly manage flare-ups to ensure a continuous supply of oxygen to the body and prevent further harm to the lungs.
- Let's examine the symptoms, causes, risk factors, diagnosis, and treatment options for bronchiectasis.
Get a second opinion from trusted experts and makeconfident, informed decisions.
Get Second Opinion
What are the Symptoms of Bronchiectasis?
Bronchiectasis disease signs and symptoms develop and change over time. They are as follows:
- The first common symptom is a continuous chronic cough and phlegm production; the excess mucus is normally clear but can become bloody if the bronchial wall is injured. Also, when an infection is present, mucus may become green or yellow.
- Chronic coughing with mucus production increases as the condition worsens, and the person generally feels increasingly exhausted and has short breaths due to mild to moderate airflow obstruction as lung function declines.
- Some people may develop wheezing, while others may lose weight due to increased breathing efforts.
- In a few cases, the symptoms of a primary condition, such as pneumonia, hide the signs and symptoms of bronchiectasis, thus making it more difficult to identify this respiratory infection.
What are the Causes of Bronchiectasis?
Bronchiectasis disease is a lung condition mainly caused by chronic airway infection causing inflammation. It is characterized by any airflow limitation, due to growth or a noncancerous tumour. In a few cases, it develops in childhood after suffering from a severe lung infection or inhaling food particles or a foreign object. Although it's mostly linked with cystic fibrosis, bronchiectasis can be caused by many other conditions, including:
- Autoimmune disorder
- Immunodeficiency syndromes
- COPD and alpha-1 antitrypsin deficiency
- Diseases that impact the cilia, which are the tiny, hair-like coverings that cover the airways and have the primary function of mucus clearance.
- Crohn's disease and ulcerative colitis.
- Allergic bronchopulmonary aspergillosis
- Chronic pulmonary aspiration
Find Our Specialists
What are the Risk factors of Bronchiectasis?
People suffering from conditions such as lung damage or lung infections are at risk of bronchiectasis. Also, there are many risk factors including:
- Severe or recurring lung infections, such as pneumonia, tuberculosis, or whooping cough
- Allergic bronchopulmonary aspergillosis
- Alpha-1-antitrypsin deficiency
- Cystic fibrosis
- Conditions that impact the cilia, which are tiny hair-like growths in the bronchi that filter mucus.
- HIV/AIDS and other immunodeficiency illnesses.
- Crohn's disease and ulcerative colitis
- Humoral immunodeficiency
- Rheumatic disorders such as rheumatoid arthritis and Sjogren's syndrome Chronic pulmonary aspiration
- Breathing in harmful substances like gases, smoke, pollutants, or coal dust.
What are the Complications of Bronchiectasis?
Bronchiectasis complications include:
- Recurring of infections
- Pulmonary bleeding
- Disruption of the respiratory system results in low oxygen levels.
- Atelectasis or a collapsed lung that makes breathing difficult.
- Low oxygen levels in the blood cause heart failure.
Some of these complications are potentially fatal. If a bronchiectasis patient notices any of the above changes, they should consult a doctor.
How to do a Bronchiectasis Diagnosis?
Bronchiectasis cannot be diagnosed with a single test. Even in its later stages, the disease's symptoms are similar to those of other conditions; therefore, it is important to rule out other conditions. The following are the most widely used diagnostic tests to detect bronchiectasis:
- A chest X-ray of the lungs is performed to look for signs of infection and scarring of the airway walls.
- Chest CT scan to provide a computer-generated image of the lungs, airways and other surrounding tissues.
- Blood tests are used to diagnose diseases or conditions that might cause bronchiectasis. Sputum culture for bacteria, fungus, or TB detection.
- Lung function tests are used to determine how well the lungs breathe air in and out. Sweat test or other tests for cystic fibrosis.
What are the Treatments for Bronchiectasis?
Generally, there’s no cure for bronchiectasis disease, but treatment is important to help manage the condition. The main aim of treatment is to reduce respiratory infections and bronchial mucus secretions. The treatment options for bronchiectasis include:
- Chest physiotherapy or chest physical therapy (CPT): A high-frequency chest wall oscillation vest is used in chest physiotherapy to help eliminate mucus from the lungs. The vest gradually compresses and releases pressure from the chest, causing coughing to loosen mucus from the bronchial tube walls.
- Antibiotics: Antibiotics are the main treatment options for recurrent lung infections due to bronchiectasis. Oral antibiotics are preferred to treat these infections. For serious infections, the doctor may prescribe intravenous (IV) antibiotics.
- Draining secretions: Another treatment is gravity-assisted drainage of bronchial secretions. A respiratory therapist can teach patients coughing strategies to help get rid of the extra mucus.
- Treating underlying conditions: If underlying illnesses such as immunological disorders or COPD are causing bronchiectasis, the doctor will treat those conditions also.
- Hydration: The doctor may advise drinking plenty of fluids, especially water, to help stop airway mucus from becoming thick and sticky. Staying hydrated helps keep airway mucus slippery, moist, and easier to cough up.
Frequently Asked Questions
No, bronchiectasis can't be completely cured, but you can manage it with treatment to feel better.
Bronchiectasis and COPD are different lung problems, and they can be bad in their ways. It varies from person to person, so ask your doctor for advice.
Lungs may not fully heal, but with treatment and healthy habits, you can make them work better and prevent more damage.
Yes, TB can lead to bronchiectasis because it can hurt your airways, and this damage can stick around even after TB is gone.
To feel better, avoid foods that can make mucus or symptoms worse, like dairy, sugary stuff, and greasy foods. It's good to drink water and eat balanced, healthy foods. For personalized advice, talk to your doctor or a dietitian.