What is orchiopexy surgery?
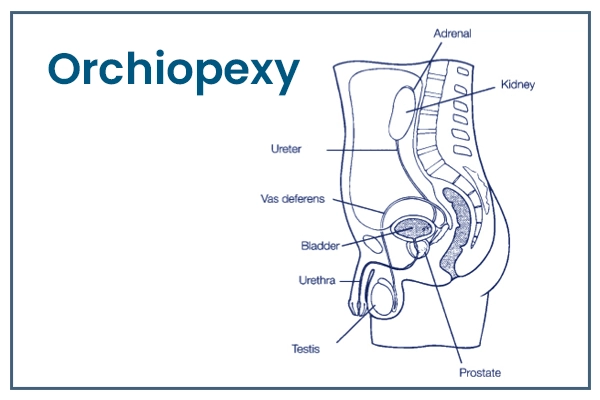
Orchiopexy surgery, also known as orchidopexy or testicular fixation, is a surgical procedure performed to treat a condition known as an undescended testicle (cryptorchidism). Cryptorchidism is a common congenital condition where one or both testicles fail to descend into the scrotum from the abdomen during fetal development. Orchiopexy is a corrective procedure aimed at bringing the undescended testicle(s) int o the scrotum and securing it properly.
Understanding Orchiopexy Surgery
Orchiopexy is typically performed in male infants or young children to address undescended testicles. The procedure is essential for several reasons:
- Preservation of Testicular Health: Undescended testicles are at a higher risk of complications, including infertility and an increased risk of testicular cancer. Orchiopexy helps preserve testicular function and health.
- Aesthetic and Functional Reasons: Positioning the testicles within the scrotum is essential for proper development, function, and appearance.
- Prevention of Torsion: Undescended testicles are more prone to testicular torsion, a painful condition that can compromise blood flow to the testicle. Orchiopexy reduces the risk of torsion.
Steps involved in Orchiopexy Surgery?
Orchiopexy Surgery Procedure
Here's an overview of what happens during an orchiopexy surgery:
- Anesthesia: The procedure is usually performed under general anaesthesia, ensuring the patient is comfortable and pain-free during the surgery.
- Incision: The surgeon makes a small incision in the groin area or scrotum, depending on the location of the undescended testicle.
- Identifying the Testicle: The surgeon carefully locates the undescended testicle, which may be in the groin area, inguinal canal, or even higher in the abdomen.
- Mobilization and Detachment: The testicle is gently mobilized from its location. If it's attached to any surrounding structures, it's carefully detached to allow repositioning.
- Bringing the Testicle Down: The surgeon brings the testicle down into the scrotum through the incision, using gentle manipulation and techniques to ensure proper positioning.
- Fixation and Anchoring: Once the testicle is in the scrotum, it is secured using sutures or, in some cases, a mesh or particular implant to prevent future re-ascension.
- Closing Incisions: The incisions are meticulously closed using sutures, dissolvable stitches, or surgical adhesive, ensuring minimal scarring.
- Dressing and Bandaging: A dressing or bandage might be applied to protect the surgical site and provide support during the initial healing period.
- Recovery and Follow-Up: After the surgery, patients are monitored in a recovery area as they wake up from anaesthesia. Pain management medications are provided to manage any discomfort. Follow-up appointments with the surgeon are scheduled to monitor healing progress and ensure the testicle remains corrected.
- Post-Operative Care: Care instructions are provided to the patient and their caregivers. This might include guidelines on wound care, activity restrictions, and pain management.
Indications of Orchiopexy Surgery
Here are the key indications for orchiopexy:
- Cryptorchidism (Undescended Testicle): The primary indication for orchiopexy is the presence of one or both testicles that have not descended into the scrotum. This condition can affect one or both testicles and occur on either side.
- Age of the Patient: Orchiopexy is often performed on infants and young children, typically between 6 months to 1 year. Early intervention is essential to prevent potential complications and ensure proper testicular development.
- Bilateral Cryptorchidism: When both testicles are undescended, bilateral orchiopexy may be indicated to correct both testicles' positions.
- Prevention of Complications: Undescended testicles are associated with an increased risk of complications, including infertility, testicular torsion (twisting), and an elevated risk of testicular cancer. Orchiopexy helps mitigate these risks.
- Absence of Spontaneous Descent: If the testicle(s) have not descended into the scrotum by the time the child reaches the age of 6 to 12 months, surgical intervention is usually recommended.
- Unilateral Cryptorchidism: In cases where only one testicle is undescended, unilateral orchiopexy focuses on correcting the position of the affected testicle.
- Improved Aesthetic Appearance: Besides the medical benefits, orchiopexy also addresses aesthetic concerns by positioning the testicles within the scrotum, resulting in a more natural appearance.
- Facilitation of Testicular Palpation: Proper positioning of the testicles in the scrotum allows for easier monitoring and palpation, aiding in detecting abnormalities.
Who will Treat for Orchiopexy
Here are the key healthcare providers involved in treating orchiopexy:
- Pediatric Urologist: Pediatric urologists are medical doctors who specialize in diagnosing, treating, and managing urological conditions in children. They are the primary specialists who perform orchiopexy surgery. Pediatric urologists have extensive training in pediatric and urologic surgery, making them highly qualified to address conditions like cryptorchidism.
- Pediatric Surgeon: Special surgeons focus on surgical care for infants, children, and adolescents. They are skilled in performing a wide range of surgical procedures in pediatric patients, including orchiopexy.
- Pediatrician: Pediatricians are medical doctors who care for infants, children, and adolescents. While they don't typically perform surgical procedures like orchiopexy themselves, paediatricians play a crucial role in diagnosing and referring children with undescended testicles to appropriate specialists for further evaluation and treatment.
- Medical Team: Orchiopexy surgery involves a collaborative effort among various medical professionals, including anesthesiologists, nurses, and surgical assistants, to ensure the safety and success of the procedure.
Preparing for Orchiopexy Surgery
Here's a guide on how to prepare:
- Consultation with Pediatric Urologist: Start by consulting a pediatric urologist or a pediatric surgeon. They will assess the child's condition, discuss the need for surgery, and provide information about the procedure.
- Medical Evaluation: The healthcare provider will thoroughly evaluate the child's overall health and any relevant medical history. This assessment helps ensure the child is fit for surgery.
- Open Communication: Provide accurate information about the child's medical history, any medications they are taking, allergies, and previous surgeries. This information is essential for the child's safety during surgery.
- Fasting Instructions: Typically, the child will need to fast (not eat or drink) for a certain period before the surgery. Follow the fasting instructions provided by the healthcare provider.
- Medication Review: Inform the healthcare provider about the child's medications. Some medicines need to be adjusted or temporarily stopped before surgery.
- Discuss Anesthesia: If the child has any concerns or fears about anaesthesia, discuss them with the healthcare provider. They can provide information to alleviate any worries.
- Hygiene and Preoperative Care: Follow any specific hygiene or preoperative care instructions provided by the healthcare provider. This might include bathing the child before the surgery.
Recovery After Orchiopexy Surgery
Recovery after orchiopexy surgery, orchidopexy, is a critical phase that requires proper care and attention to ensure the child's comfort, healing, and well-being. While individual experiences may vary, here's a general overview of what you can expect during the recovery period:
- Immediate Post-Operative Phase: After the surgery, the child will be monitored in a recovery area as they wake up from anaesthesia . Pain management medications will be administered to ensure the child's comfort.
- Discharge from the Hospital: Once the child is alert and stable and the healthcare team is satisfied with their condition, they will be discharged from the hospital or surgical centre.
- Pain and Discomfort: Some discomfort, swelling, and bruising in the surgical area are expected after surgery. The healthcare provider will prescribe pain medications or recommend over-the-counter pain relievers to manage discomfort.
- Dressing and Bandages: The surgical area may be covered with a dressing or bandage to protect it and provide support during the initial healing period. Follow any dressing care instructions provided by the healthcare provider.
- Activity Restrictions: The child should avoid strenuous activities, heavy lifting, and vigorous exercise for a certain period, usually a few weeks. Engaging in such activities too soon can disrupt the healing process.
- Follow-Up Appointments: Scheduled follow-up appointments with the pediatric urologist or surgeon are essential for monitoring the child's healing progress. During these appointments, the healthcare provider will assess the surgical site, remove sutures, and address concerns.
- Hygiene and Wound Care: Follow the healthcare provider's guidelines for keeping the surgical area clean and dry. Avoid submerging the surgical site in water until advised by the healthcare provider.
Lifestyle Changes After Orchiopexy Surgery
After undergoing orchiopexy surgery, also known as orchidopexy, specific lifestyle changes and considerations can contribute to smoother recovery and optimal healing for the child. While these changes are generally temporary, they ensure the surgical area heals appropriately and minimizes discomfort. Here are some lifestyle changes to consider:
- Gentle Handling: Encourage the child to avoid touching or manipulating the surgical area to prevent disruption of the healing process. Handle the area gently when helping the child with dressing changes or hygiene routines.
- Physical Activities: The child should avoid engaging in vigorous physical activities, sports, and rough play during the initial recovery period. Gradually reintroduce regular activities based on the healthcare provider's guidance.
- Bathing and Hygiene: Follow the healthcare provider's instructions for keeping the surgical area clean and dry. Be cautious while bathing the child, ensuring that water only directly contacts the surgical site once the healthcare provider approves it.
- Clothing Choices: Choose loose, comfortable clothing that won't rub against or irritate the surgical area. Avoid clothing with zippers, buttons, or tight waistbands that might cause discomfort.
- Physical Contact: Advise the child to be cautious when engaging in physical contact with others, especially in the area of the surgery. Educate them about gentle play to avoid accidental injury to the surgical site.
- School and Activities: Depending on their comfort level, the child can generally return to school a few days after the surgery. If necessary, inform the school staff about the recent surgery to ensure appropriate care.
- Follow-Up Appointments: Ensure the child attends all scheduled follow-up appointments with the pediatric urologist or surgeon. These appointments are crucial for monitoring the healing progress and addressing any concerns.
- Healthy Diet and Hydration: Encourage the child to maintain a balanced and healthy diet to support their healing. - Drinking plenty of fluids is also essential for overall well-being.
- Rest and Sleep: Ensure the child gets sufficient rest and sleep during recovery to aid the healing process.