Understanding Calcified Lesions
There are several types of calcified lesions, each with its characteristics:
- Atherosclerotic Calcifications: Calcifications can occur in blood vessel walls due to atherosclerosis, characterized by plaque accumulation. These calcifications can contribute to narrowed or hardened arteries, potentially leading to cardiovascular issues.
- Soft Tissue Calcifications: Soft tissues like tendons, ligaments, and muscles can sometimes develop calcifications, often resulting from injuries, inflammation, or chronic conditions. These calcifications can limit mobility and cause discomfort.
- Visceral Organ Calcifications: Organs like the kidneys, lungs, and liver can develop calcifications due to various causes, including infections, inflammation, or chronic diseases.
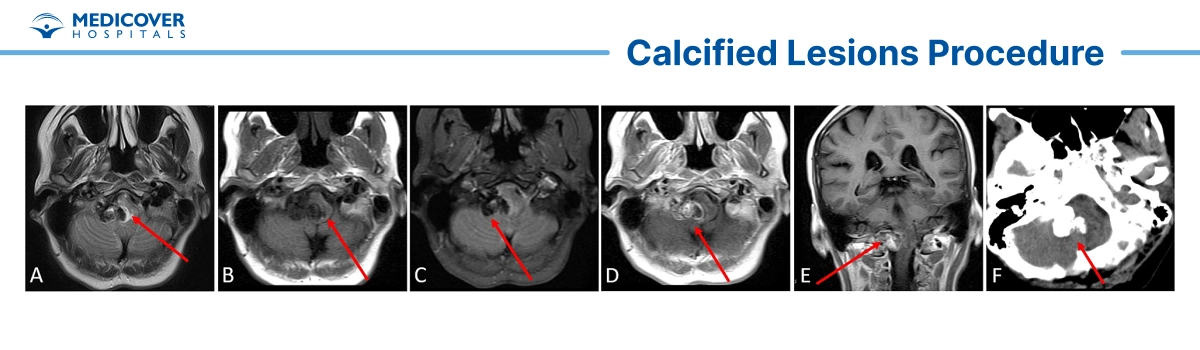
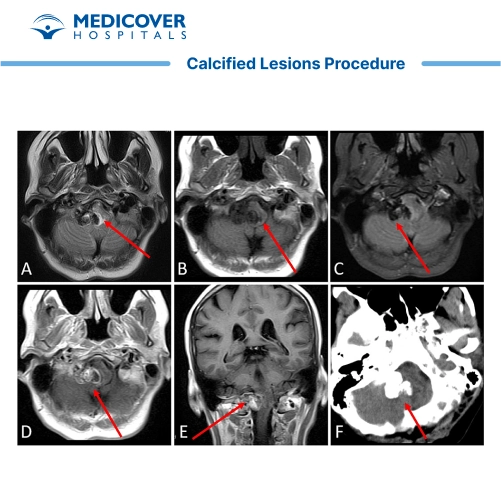
- Brain Calcifications: Calcifications can occur in the brain, which may be associated with conditions like neurodegenerative diseases, infections, or other underlying health issues.
- Dystrophic Calcifications: These calcifications can develop in areas of damaged tissue, often due to injury or localized inflammation.
- Metastatic Calcifications: Metastatic calcifications arise when there's an imbalance in calcium and phosphate levels in the body, causing calcium to deposit in tissues where it usually wouldn't accumulate.
Steps involved in Calcified Lesions?
The management and treatment approach for calcified lesions depends on the underlying cause, the location of the calcifications, and the potential impact on the individual's health. Here are some common approaches used for calcified lesions:
- Diagnostic Evaluation: If calcified lesions are detected on imaging studies, further diagnostic tests are conducted to determine the cause and nature of the calcifications. These tests may include blood tests, biopsies, and additional imaging modalities.
- Observation and Monitoring: In some cases, especially if the calcifications are small and not causing any symptoms, the healthcare provider may opt for a "watch and wait" approach. Regular monitoring through imaging studies can help track any changes over time.
- Lifestyle Modifications: Lifestyle changes can play a role in managing certain types of calcified lesions. For example, lifestyle modifications may be recommended for individuals with atherosclerotic calcifications to improve heart health and manage risk factors like high blood pressure and cholesterol levels.
- Medications: Depending on the underlying condition, medications may be prescribed to manage symptoms, reduce inflammation, prevent further calcification, or address related health issues.
- Physical Therapy and Rehabilitation: For calcifications in soft tissues or around joints, physical therapy and rehabilitation exercises may be recommended to improve mobility, alleviate pain, and prevent complications.
- Surgical Removal: Surgical removal of calcified lesions may be considered if they are causing significant discomfort, impairing organ function, or posing a health risk. This approach is often used for more extensive or symptomatic calcifications.
- Treatment of Underlying Conditions: Addressing the underlying cause of calcifications is essential. If calcifications result from an underlying condition such as an infection or inflammatory disease, treating the underlying cause can help prevent further calcification.
- Medications to Manage Calcium Levels: In cases of metastatic calcifications, medications may be prescribed to regulate calcium and phosphate levels in the body, preventing further deposition in tissues.
Indications of Calcified Lesions?
Calcified lesions can develop for various reasons and in different body parts. The presence of calcifications might indicate an underlying health issue or condition. Here are some signs and potential underlying causes of calcified lesions in various contexts:
- Cardiovascular System: Atherosclerotic calcifications in blood vessels can indicate atherosclerosis, a condition characterized by plaque buildup on artery walls. This can increase the risk of heart disease, stroke, and other cardiovascular issues.
- Soft Tissues and Joints: Calcifications in soft tissues, tendons, ligaments, or joints might indicate injuries, chronic inflammation, or conditions like tendinitis, bursitis, or calcific shoulder periarthritis.
- Organs: Calcifications in visceral organs like the kidneys, liver, lungs, or pancreas could be associated with infections, chronic diseases (such as cirrhosis or kidney disease), or other underlying conditions.
- Brain and Nervous System: Brain calcifications can be linked to neurodegenerative disorders, infections (such as toxoplasmosis), or metabolic conditions like Fahr's disease.
- Breast Tissue: Calcifications in breast tissue can indicate benign breast conditions or, in some cases, early signs of breast cancer. Mammograms are used to monitor and assess these calcifications.
- Skin: Calcified lesions on the skin might result from conditions like calcinosis cutis, which involves the deposition of calcium salts in the skin due to various underlying factors.
- Soft Tissue Sarcomas: Calcifications in soft tissue masses can sometimes indicate the presence of a soft tissue sarcoma, a type of cancer.
- Dental and Oral Health: Calcifications in oral tissues can be related to dental calculus (tartar) or conditions affecting the salivary glands.
- Blood Vessels and Heart Valves: Calcifications in blood vessels or heart valves might indicate conditions like vascular calcification or valvular heart disease.
Who will treat for Calcified Lesions?
Treating calcified lesions involves a multidisciplinary approach, with various healthcare professionals collaborating to address the underlying causes, manage symptoms, and develop an effective treatment plan. The specific medical specialists involved can vary depending on the location of the calcified lesion, the underlying condition, and the individual's health needs. Here are some of the healthcare professionals who may be involved in treating calcified lesions:
- Primary Care Physicians: Primary care doctors, such as family or internal medicine physicians, maybe the initial point of contact. They can assess your symptoms, order initial tests, and refer you to specialists.
- Orthopedic Surgeons: Orthopedic surgeons specialize in the diagnosis and treatment of musculoskeletal conditions, which can include calcified lesions affecting bones, joints, tendons, and ligaments.
- Rheumatologists: Rheumatologists specialize in autoimmune and inflammatory disorders. They may be involved in calcifications resulting from rheumatoid arthritis or systemic sclerosis.
- Cardiologists: Cardiologists specialize in heart and cardiovascular health. They may be consulted for calcifications in blood vessels, heart valves, and other cardiovascular structures.
- Nephrologists: Nephrologists are kidney specialists who can provide insights and treatment for calcifications in the kidneys or urinary system.
- Pulmonologists: Pulmonologists specialize in lung and respiratory conditions. They may be consulted for calcified lesions in lung tissue or airways.
- Neurologists: Neurologists specialize in the nervous system. They can be involved in calcifications in the brain or nervous system.
- Gastroenterologists: Gastroenterologists specialize in digestive system health. They may be consulted for cases involving calcifications in the gastrointestinal tract or related organs.
- Oncologists: Oncologists specialize in cancer treatment. They may be consulted for calcifications associated with malignancies or cancerous growths.
- Obstetricians and Gynecologists: In cases where calcified lesions are found in the breast tissue, gynaecologists and breast surgeons can provide evaluation and treatment options.
- Dermatologists: Dermatologists specialize in skin health. They can diagnose and treat calcified lesions on the skin.
- Dentists and Oral Surgeons: For calcifications related to oral health, dentists and oral surgeons can provide assessment and treatment options.
- Endocrinologists: Endocrinologists specialize in hormonal and metabolic disorders. They may be involved in cases of metabolic calcifications.
- Infectious Disease Specialists: Infectious disease specialists can provide diagnosis and treatment for cases where calcifications are due to infections.
- Radiologists: Radiologists play a critical role in diagnosing calcified lesions through imaging studies and providing insights to other specialists.
- Physical Therapists: Physical therapists can help with rehabilitation, pain management, and improving mobility after treatment for calcified lesions.
Preparing for Calcified Lesions?
Preparing for evaluating and managing calcified lesions involves gathering information, understanding the process, and ensuring you're ready for medical appointments and potential treatments. Here are steps to help you prepare:
- Gather Medical Information: Collect your medical records, including past diagnoses, medications, surgeries, and any relevant family medical history. This information will help your healthcare provider understand your overall health.
- List Symptoms and Concerns: List any symptoms you're experiencing and any concerns or questions you have about the calcified lesion. This will ensure you cover all your points during your appointments.
- Research Healthcare Providers: If you have yet to be referred to a specialist, research and find healthcare providers specializing in the relevant field (e.g., orthopaedics, cardiology, dermatology). Look for providers with expertise in treating calcified lesions.
- Schedule Appointments: Schedule appointments with your chosen healthcare providers. Discuss your situation and ask your primary care physician for referrals if needed.
- Write Down Questions: Write down a list of questions to ask your healthcare providers during appointments. This can include questions about the nature of the lesion, possible causes, treatment options, and potential outcomes.
- Prepare Relevant Documents: Bring copies of your medical records, test results, and imaging studies (X-rays, MRIs, etc.) to your appointments. This will provide valuable information for your healthcare provider.
- Review Your Medications: List all your medications, supplements, and vitamins. Please share this list with your healthcare providers to ensure they have a complete picture of your medical history.
- Prepare for Diagnostic Tests: If your healthcare provider orders diagnostic tests, such as blood tests, biopsies, or imaging studies, follow any preparation instructions provided. This might include fasting before a blood test or wearing appropriate clothing for an imaging study.
- Ask About Treatment Options: During your appointments, ask your healthcare provider about the available treatment options, potential risks, benefits, and expected outcomes.
Recovery after Calcified Lesions?
The recovery process after treatment for calcified lesions can vary depending on factors such as the location of the lesion, the underlying condition, and the type of treatment received. Here are some general considerations for recovery:
- Follow Medical Recommendations: Following your healthcare provider's post-treatment instructions is crucial. This might include wound care, medication schedules, and activity restrictions.
- Rest and Recovery: Depending on the treatment, you may need to rest and limit physical activity. Give your body the time it needs to heal.
- Pain Management: If you experience pain or discomfort after treatment, your healthcare provider may prescribe pain medications or recommend over-the-counter options.
- Wound Care: If your treatment involves an incision or wound, follow your healthcare provider's instructions for cleaning and dressing the wound to prevent infection and promote healing.
- Physical Therapy: In cases where the lesion affected mobility or function, your healthcare provider may recommend physical therapy to help restore strength, flexibility, and functionality.
- Rehabilitation Exercises: Depending on the location of the lesion and the type of treatment, you might be prescribed rehabilitation exercises to regain strength and mobility.
- Follow-Up Appointments: Attend all scheduled follow-up appointments with your healthcare provider. These appointments allow them to monitor your progress, assess healing, and address concerns.
- Manage Symptoms: If you experience new or worsening symptoms after treatment, contact your healthcare provider promptly. They can help determine whether it's a normal part of recovery or requires further attention.
- Gradual Return to Normal Activities: As you recover, gradually reintroduce activities into your routine as your healthcare provider advises. Avoid overexertion and listen to your body.
Lifestyle Changes after Calcified Lesions procedure
Lifestyle changes after undergoing treatment for calcified lesions can significantly support your recovery, prevent recurrence, and maintain overall health. These changes might vary depending on the location of the lesion, the underlying condition, and the treatment received. Here are some general lifestyle adjustments to consider:
Dietary Modifications:
- Follow a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Reduce the consumption of processed foods, sugary snacks, and excessive amounts of salt.
- If you have conditions like atherosclerosis, focus on heart-healthy foods to support cardiovascular health.
Hydration:
Drink adequate water throughout the day to stay hydrated and support overall bodily functions.
Physical Activity:
- Engage in regular physical activity as recommended by your healthcare provider.
- Consult a physical therapist to develop a safe and effective exercise routine if your treatment involves orthopaedic issues.
Smoking Cessation:
If you smoke, consider quitting smoking, as it can contribute to various health issues, including cardiovascular problems and impaired healing.
Alcohol Consumption:
If you consume alcohol, do so in moderation. Excessive alcohol intake can have adverse effects on your health and recovery.
Stress Management:
Practice stress-reduction techniques such as deep breathing, meditation, yoga, or mindfulness to support your overall well-being.
Weight Management:
Maintain a healthy weight through balanced eating and regular physical activity.
Medication Adherence:
If prescribed medications to manage an underlying condition, adhere to the recommended dosages and schedules.
Regular Check-ups:
Attend follow-up appointments with your healthcare provider to monitor your recovery and overall health.
Infection Prevention:
Follow good hygiene practices to prevent infections, especially if you have an open wound or surgical procedure.