Central Airway Obstruction
July 20 2022 Medicover Hospitals | KakinadaCentral airway obstruction refers to the obstruction of airflow in the trachea, and the main stem bronchi is apotentially life-threatening condition due to several malignant and non-malignant processes. A 38-year-old male came to our ER with symptoms of difficulty in breathing, cough, hemoptysis, difficulty in swallowing, and feeling of choking for 1 week. He had undergone surgery and radiation for squamous cell carcinoma 2years ago. On examination, he had respiratory distress with inspiratory stridor. He was admitted to the intensive care unit and was started on non-invasive ventilation support, intravenous fluids, and other supportive care. After providing general anesthesia patient was directly incubated with a rigid bronchoscope (Novatech, Tracheoscopy 14 mm O.D, Novatech SA, LaCiotat, France).
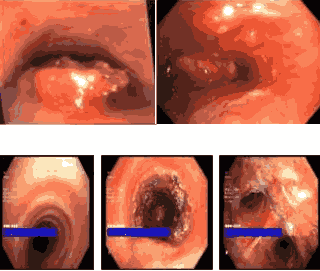
Under visualization showed extrinsic luminal compression and tumor invasion into the lumen causing total occlusion of the tracheal at mid-level.Mechanical debulking was done by coring with a rigid scope and the tumor was extracted piecemeal. Because of the extrinsic compression by the tumor, a self-expandable metallic stent (Otomed fully covered, 16x80 mm) was deployed using flexible bronchoscope guidance through a rigid scope. The patient’s condition remained normal throughout the procedure and his end-tidal carbon dioxide (EtCO2) was normal after stenting. Check bronchoscopy showed a well-positioned and expanded metallic stent in situ. Stridor and respiratory distress were completely relieved. Because of the extensive tumor burden causing lymphedema and brachial plexus compression, he was advised palliative radiotherapy. He has been on follow-up for 2 months with improved quality of life post debulking and stenting.
Case Report
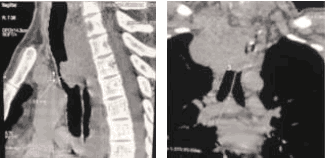
Here we present a case of central airway obstruction due to a tracheal tumor, managed successfully at Medicover Hospitals, Kakinada. A 38-year-old male came to our ER with symptoms of difficulty in breathing, cough, hemoptysis, difficulty in swallowing, and feeling of choking for one week. He had a history of squamous cell carcinoma esophagus for which he underwent surgery and radiation 2 years ago. He does not have any lifestyle habits. On examination, he has been in respiratory distress with inspiratory stridor. His general condition is poor, and his psychological condition is very low. His vitals at presentation were: blood pressure- 100/60, temperature- 99 F, respiratory rate- 28/min, oxygen saturation- 94% on room temperature, and pulse rate- 120/min. Immediate CT chest done showed upper mediastinal growth around the esophagus extending anteriorly causing near-complete occlusion of the tracheal lumen (>80). Arterial blood gas (ABG) showed respiratory alkalosis.
He was admitted to the intensive care unit and started on non-invasive ventilation support, intravenous fluids, and other supportive care. Given the advanced nature of the disease and bad prognostic signs, the family was counseled and clearly explained the patient’s condition and expected outcome. An immediate multidisciplinary team discussion had been called for, including a surgical oncologist, cardiothoracic surgeon, radiation oncologist, medical oncologist, anesthetist, intensivist, and pulmonologist. The patient and his family decided to take an aggressive approach and opted not to leave any stone unturned. So, the option of immediate rigid bronchoscopy-guided debulking and stenting was decided.
Procedure
After providing general anesthesia, the patient’s head was d positioned in a "sniffing" position,and intubation was done directly with a rigid 6 Medicover Hospials - Kakinada HOSPITALS bronchoscope (Novatech, Tracheoscopy 14 mm O.D, Novatech SA, La Ciotat, France) under visualization. Thetrachea showed extrinsic luminal compression and tumor invasion into the lumen causing near-total occlusion of the trachea at mid-level. After injecting 1% adrenaline perilesional, mechanical debulking was done by scoring with rigid scope and tumor extracted piecemeal.Hemostasis was secured by the tamponade effect of tracheoscopy followed by electrocauterization of the tumor base. Near normal patency of tracheal lumen was achieved. Given extrinsic compression by the tumor, a self-expandable metallic stent (Otomed, fully covered, 16x 80 mm) was deployed using flexible bronchoscope guidance through the rigid scope.
The patient’s condition remained stable throughout the procedure and his EtCO2 normalized immediately after stenting. He was extubated on the table and maintained on oxygen support with nasal prongs. Check bronchoscopy done the next day showed a well-positioned and expanded metallic stent in situ. Stridor and respiratory distress were completely relieved and the patient went home walking on his own. Given extensive tumor burden causing lymphedema and brachial plexus compression, he was advised palliative radiotherapy. He has been under follow-up for 2 months with improved quality of life post debulking and stenting.
POPULAR POSTS
25.08.2022
Medicover Hospitals has done Liver Diseases Awareness program and Launched Liver Clinic.
24.08.2022
A baby born at 24 weeks of gestation with a less chance of survival was saved
22.08.2022
Mahabubnagar farmer recovers after complex brain surgery at Medicover Hospitals
24.06.2022
Medicover Hospitals organized “Walkathon”: An event to raise awareness on World No Tobacco Day 2022
03.06.2022
Fetal Heart Rate Problem
02.06.2022
Man with Severe Bullet Injuries from Yemen Saved at Medicover Hospitals
01.06.2022
Contributors
