What is Meningitis?
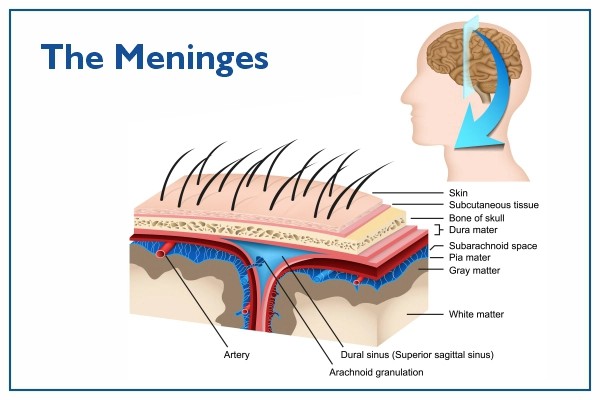
Meningitis is a potentially life-threatening infection where the protective membranes, called the meninges, surrounding your brain and spinal cord get inflamed. This inflammation can disrupt the normal functioning of the nervous system, leading to serious complications. Meningitis can be very serious and requires immediate medical attention. Most commonly, meningitis is caused by a viral or bacterial infection. Some common bacteria that cause meningitis are Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae. Fungal meningitis is less common and usually happens to people with weak immune systems.
Symptoms and Signs:
Symptoms of meningitis can vary and may appear quickly or over several days. Typically, they include:
- Fever: A high temperature is one of the first signs of meningitis.
- Severe headache: This is often different than normal headaches and is persistent.
- Stiff neck: Neck stiffness, often along with headache and fever, can be a key sign of meningitis.
- Sensitivity to light: Many people with meningitis become sensitive to bright light.
- Nausea and vomiting: This can be due to the fever and general illness.
- Confusion or difficulty concentrating: This occurs due to the infection's impact on the brain.
- Sleepiness or difficulty waking up: Meningitis can cause a person to feel extremely tired.
In babies, symptoms may be harder to notice and may include:
- High fever: It can be challenging to notice in infants, but a change in body temperature can be a sign.
- Bulging soft spot on the head: This can occur due to increased pressure from the inflammation.
- Irritability or excessive crying: Infants may become more irritable or cry more than usual.
- Poor feeding: Infants may lose their appetite or have difficulty feeding.
- Sleepiness or difficulty waking up: Babies may sleep more than usual or be challenging to wake up.
- Stiffness in the body and neck: It can be hard to detect in infants but is a serious symptom.
Causes
Meningitis can be caused by a number of different pathogens, including:
- Bacteria such as Neisseria meningitidis (meningococcal meningitis), Streptococcus pneumoniae (pneumococcal meningitis), and Haemophilus influenzae (Hib meningitis). Bacterial meningitis is generally more severe and can be life-threatening.
- Viruses like enteroviruses, herpes viruses (especially Herpes Simplex Virus-2), and others. Viral meningitis, while uncomfortable, is usually less severe than bacterial meningitis and individuals typically recover on their own with proper rest and care.
- Fungi, like Cryptococcus, are less common causes and are typically seen in people with weakened immune systems. Fungal meningitis is severe and requires immediate treatment.
- Rarely, parasites or certain medications or diseases can also cause meningitis.
Who is at risk of getting Meningitis?
Meningitis can occur in anyone, but some groups have a higher risk:
- Infants and young children: Children under age 5, especially infants, are at increased risk due to their developing immune system.
- Teenagers and young adults: People between 15 and 24 years old are also at higher risk, especially those living in communal settings like dormitories or military bases.
- Older adults (over 65 years): The immune system weakens with age, increasing the risk of infections.
- People with a weak immune system: This includes people undergoing chemotherapy, those on immunosuppressive medications, and those with chronic diseases such as diabetes or HIV.
Red flag sings/Warning Signs:
The red flags that indicate the need for immediate medical attention are:
- Seizures: These are caused by electrical disturbances in the brain and could indicate a serious condition like meningitis.
- Severe headache with high fever: This combination of symptoms could indicate a serious infection, such as meningitis.
- A rash that doesn't fade when you press a glass against it: This could indicate septicemia (a type of blood poisoning), a life-threatening complication of meningitis.
It's important to note that these warning signs can develop rapidly, even within a matter of hours. If you or a loved one experiences any of these signs, seek immediate medical attention.
Spread
Meningitis spreads from person to person through various means:
- Close contact with an infected person: This can include activities like coughing, sneezing, or kissing where respiratory droplets are exchanged.
- Sharing utensils or personal items: The germs causing meningitis can live on surfaces and can spread if you use someone else’s utensils, toothbrush, or other personal items.
- During childbirth: A pregnant woman with bacterial meningitis can pass the infection to her baby during birth.
Prevention
Prevention strategies for meningitis include:
- Vaccinations: Meningococcal, Pneumococcal, and Hib vaccines can protect against some of the most common bacterial causes of meningitis. Vaccinations are a crucial preventive measure, especially for those at higher risk.
- Hand hygiene: Regular hand washing with soap and water or using a hand sanitizer can help stop the spread of infectious germs that can cause meningitis.
- Avoiding close contact with sick individuals: Keeping a safe distance from people who are sick can prevent the spread of the germs that cause meningitis.
Diagnosis
Doctors diagnose meningitis using several methods:
- Physical examination: The doctor will look for signs of infection, such as a rash or a stiff neck. They may also test for Brudzinski's and Kernig's signs, two clinical signs often used to suggest the presence of meningitis.
- Blood tests: Blood cultures can be used to identify the bacteria or virus causing the infection. Other blood tests can give clues about the body's response to an infection.
- Lumbar puncture (spinal tap): This involves taking a sample of cerebrospinal fluid (CSF), which surrounds the brain and spinal cord. This fluid can be examined to identify the type of meningitis.
- Brain imaging: In some cases, a CT Scan or MRI scan may be done to check for complications such as swelling or abscesses.
Differential Diagnosis/Conditions mimicking Meningitis
Several other conditions can mimic the symptoms of meningitis, making diagnosis challenging:
- Encephalitis: This is inflammation of the brain itself, often caused by a viral infection. It can cause fever, headache, confusion, and seizures, just like meningitis.
- Brain abscess: This is a pocket of infection in the brain, which can cause headache, fever, and other neurological symptoms similar to meningitis.
- Severe flu or other respiratory infections: These can cause high fever, headache, and body aches, which may initially seem like meningitis.
- Subarachnoid hemorrhage: This condition, often caused by a ruptured aneurysm, can cause a severe headache and neck stiffness, mimicking meningitis.
- Guillain-Barre Syndrome and other neurologic conditions: These conditions can cause symptoms that overlap with meningitis, such as weakness and sensory changes.
Your doctor will need to rule out these and other conditions to confirm a diagnosis of meningitis.
Treatment
Treatment for meningitis depends on the underlying cause:
- Bacterial meningitis is a medical emergency and is treated with intravenous antibiotics and sometimes corticosteroids. This helps to ensure the bacteria are killed off quickly and reduces the risk of complications.
- Viral meningitis usually improves on its own within a week or two, but hospital admission may be needed for close monitoring. Antiviral medication may be used for certain viruses, like herpes simplex virus.
- Fungal meningitis is treated with long courses of high-dose antifungal medications. This type of meningitis is less common and usually only affects people with weakened immune systems.
Dos and Don’ts
| Do’s | Don’ts |
| Do get vaccinated: Vaccines can protect you from many types of meningitis. This is especially important for those at higher risk. | Don't ignore the symptoms: Meningitis can progress rapidly, so it's crucial to seek help promptly. If you suspect meningitis, seek immediate medical attention. |
| Do maintain good hygiene: Wash your hands regularly with soap and water, especially before eating and after using the toilet. Also avoid sharing personal items like utensils, toothbrushes, and drinking glasses. | Don't come in close contact with a person diagnosed with meningitis: The disease can be contagious, and close contact could put you at risk. |
| Do seek medical help promptly if you suspect meningitis: Early treatment is vital and can save lives. Don't wait until the symptoms get severe. | Don't skip vaccinations: They are a crucial preventive measure against various types of meningitis. |
Frequently Asked Questions
1. When should I approach a doctor immediately?
If you or your loved one is experiencing symptoms like a severe headache, high fever, stiff neck, or a rash that doesn't fade when pressed with a glass, you should seek medical attention immediately. These symptoms could indicate a serious condition like meningitis that needs prompt treatment. If a person is sleeping or difficult to wake up, or if they show signs of confusion or irritability, these are also reasons to seek immediate medical help.
2. Can one get meningitis more than once?
Yes, it's possible to get meningitis more than once, as there are different types of bacteria, viruses, and fungi that can cause the disease.
3. What type of doctors treat meningitis?
Infectious disease specialists and neurologists often treat meningitis. In severe cases, critical care specialists may also be involved in the patient's care.
Remember, meningitis is a serious condition, and prompt medical attention can save lives. If you suspect that you or someone else might have meningitis, don't delay—seek medical help immediately.
