Indications of Chemotherapy
Chemotherapy is indicated for various medical conditions, with cancer being the most common reason. It's often recommended in the following situations:
- Primary Cancer Treatment: Chemotherapy can be the main treatment for certain types of cancer, especially when surgery or radiation therapy is not feasible.
- Adjuvant Therapy: After surgery or radiation, chemotherapy may be used to eliminate any remaining cancer cells and reduce the risk of recurrence.
- Neoadjuvant Therapy: Administered before surgery or radiation to shrink tumors and make them more manageable for subsequent treatment.
- Metastatic Cancer: Chemotherapy is employed to control the growth of cancer that has spread to other parts of the body.
- Palliative Care: In advanced or terminal cases, chemotherapy can alleviate symptoms, improve quality of life, and extend survival.
- Hematologic Diseases: Chemotherapy treats blood-related disorders like leukemia,lymphoma, and multiple myeloma
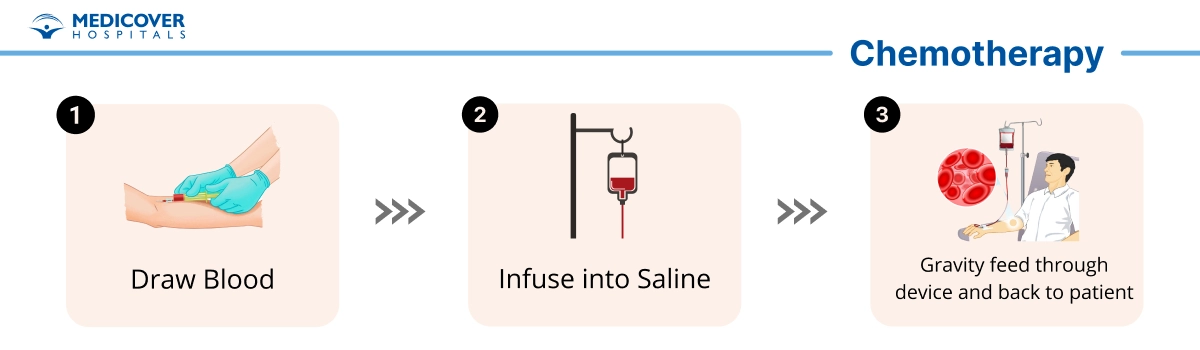
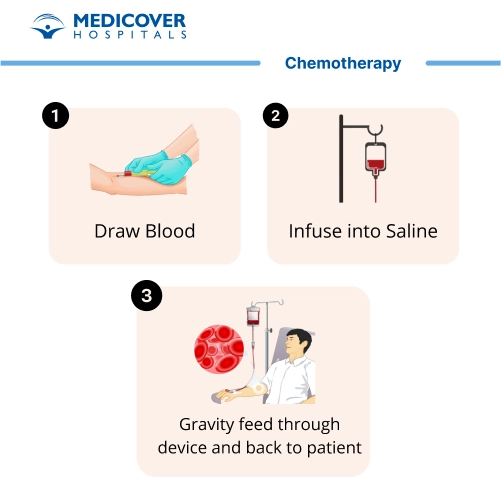
Steps in Chemotherapy procedure
Chemotherapy is a treatment approach commonly used to treat cancer by using medications to target and destroy cancer cells or slow their growth. The specific steps involved in a chemotherapy procedure can vary based on the type of cancer, the chemotherapy drugs being used, and the patient's individual needs. However, here are the general steps involved in a chemotherapy procedure:
- Medical Assessment and Consultation: Before starting chemotherapy, the patient undergoes a thorough medical assessment, including physical exams, blood tests, imaging scans, and possibly a biopsy. This helps determine the type, stage, and extent of the cancer.
- Treatment Planning: Based on the assessment, oncologists develop a personalized treatment plan that outlines the chemotherapy drugs, dosage, schedule, and duration of treatment. This plan takes into account the patient's overall health, cancer type, and any other medical conditions.
- Access Placement: In some cases, a central venous catheter (such as a port or catheter) may be surgically implanted under the skin or into a large vein, usually in the chest. This access device provides a more convenient and comfortable way to administer chemotherapy drugs and take blood samples.
- Preparation for Treatment: On the day of treatment, the patient arrives at the treatment center or hospital and may need to provide a blood sample for additional tests. The medical team ensures the patient's eligibility for chemotherapy on that particular day.
- Administration of Chemotherapy:
- Chemotherapy drugs are administered through various methods, including intravenous (IV) infusion, oral pills, injections, and sometimes even topical applications.
- During IV infusion, the drugs are delivered through a needle inserted into a vein, and the process can take several hours. Patients may receive chemotherapy in a treatment room while being monitored by medical staff.
- Monitoring and Support:
- Throughout the administration of chemotherapy, medical professionals closely monitor the patient's vital signs, potential side effects, and overall well-being.
- Patients might receive fluids, medications to manage side effects, and other supportive care as needed.
- Completion of Treatment Session: Once the chemotherapy drugs have been fully administered, the patient may need some additional time for observation to ensure there are no immediate adverse reactions.
- Recovery and Follow-Up:
- After the treatment session, patients may be able to return home, or they might need to stay in the hospital overnight depending on the chemotherapy regimen.
- Patients are given instructions on managing potential side effects, staying hydrated, taking prescribed medications, and maintaining a healthy lifestyle during chemotherapy.
- Subsequent Treatment Sessions: Chemotherapy is often administered in cycles, with treatment sessions followed by rest periods to allow the body to recover. The number of cycles and the frequency of treatment sessions depend on the specific treatment plan.
- Ongoing Monitoring and Adjustments:
- Throughout the course of chemotherapy, the patient's response to treatment is monitored through regular check-ups, blood tests, imaging scans, and discussions with the oncologist.
- The treatment plan may be adjusted based on how the patient is responding to chemotherapy and any changes in their overall health.
Who will Treat for Chemotherapy procedure
Chemotherapy procedures are typically administered and overseen by a team of medical professionals, including:
- Medical Oncologists: These are doctors specialized in oncology (the study and treatment of cancer). They develop the treatment plan, choose the appropriate chemotherapy drugs, and oversee the entire course of chemotherapy.
- Nurse Practitioners and Physician Assistants: These healthcare professionals work closely with medical oncologists to administer chemotherapy, monitor patients' reactions, and provide supportive care.
- Oncology Nurses: These specialized nurses have training in administering chemotherapy, managing side effects, and providing emotional support to patients during treatment.
- Pharmacists: Oncology pharmacists prepare and dispense chemotherapy drugs, ensuring accurate dosing and compatibility with other medications.
- Oncology Social Workers: These professionals offer emotional and practical support to patients and their families, helping them cope with the challenges of chemotherapy and its effects.
- Nutritionists/Dietitians: These experts provide guidance on maintaining proper nutrition during chemotherapy to support the body's healing process.
- Radiation Oncologists: In some cases, chemotherapy may be combined with radiation therapy. Radiation oncologists specialize in using radiation to treat cancer.
- Support Staff: Hospital and clinic staff play a crucial role in creating a comfortable and safe environment for patients during chemotherapy sessions.
Preparing for a Chemotherapy procedure
Preparing for chemotherapy involves a combination of physical and emotional readiness to ensure the best possible experience during treatment. Here's a guide on how to prepare:
- Understand the Treatment: Discuss the chemotherapy plan with your medical oncologist. Understand the purpose, duration, and potential side effects of the treatment.
- Plan Ahead: Arrange transportation for your appointments, as you might feel fatigued or unwell after sessions.
- Nutrition and Hydration: Maintain a balanced diet and stay hydrated before treatment. Consult a dietitian for guidance on foods that support your health during chemotherapy.
- Medication Review: Inform your healthcare team about all medications, supplements, and vitamins you're taking. Some medications might interfere with chemotherapy.
- Blood Tests: You may need blood tests to assess your overall health and blood cell counts before starting chemotherapy.
- Emotional Support: Seek emotional support from loved ones, friends, or support groups to help you cope with the upcoming challenges.
- Rest and Exercise: Get enough rest before treatment, and engage in gentle exercise to maintain physical strength.
- Address Dental Issues: Visit your dentist for any necessary dental work before starting chemotherapy. Dental problems can be exacerbated during treatment.
- Skin and Nail Care : Ensure good hygiene and address any skin or nail concerns before treatment. Chemotherapy can affect these areas.
- Dress Comfortably: Wear loose-fitting, comfortable clothes to your appointments, as you might be sitting for an extended period.
- Arrange Accompaniment: If possible, have a family member or friend accompany you to appointments for emotional support.
- Organize Personal Items : Bring items like reading material, headphones, or music to keep you occupied during treatment.
- Be Informed: Learn about potential side effects and strategies to manage them. Ask your medical team about what to expect.
- Mental Preparation: Mentally prepare for the treatment process by maintaining a positive outlook and addressing any fears or anxieties.
- Clear Schedule : Keep your schedule as free as possible during treatment days to minimize stress.
- Contact Information: Have contact information for your medical team readily available in case you have questions or concerns.
Recovery after Chemotherapy procedure
Recovery after a chemotherapy procedure can vary depending on the specific drugs used, your overall health, and your body's response to treatment. Here's what you might experience during the recovery period:
- Immediate Effects : Right after the chemotherapy session, you might feel tired, dizzy, or lightheaded. These immediate effects usually subside within a few hours.
- Nausea and Vomiting : Some people experience nausea and vomiting within a few hours to days after treatment. Your healthcare team might prescribe anti-nausea medications to help manage these symptoms.
- Fatigue : Fatigue is a common side effect of chemotherapy. Give yourself permission to rest and conserve energy as needed.
- Weakness and Muscle Aches : You might feel weak or experience muscle aches. Gentle stretches and light exercise can help alleviate these discomforts over time.
- Changes in Appetite : Your appetite might fluctuate during recovery. Aim for a balanced diet to support your body's healing process.
- Immune System Impact : Chemotherapy can temporarily weaken your immune system, making you more susceptible to infections. Follow your healthcare team's guidance to minimize infection risk.
- Hair Loss : Depending on the drugs used, you might experience hair loss. This can start a couple of weeks after treatment. Remember that hair usually grows back after chemotherapy is completed.
- Emotional Changes : Coping with the physical and emotional challenges of chemotherapy can impact your mood. Seek support from loved ones, friends, or mental health professionals if needed.
- Monitoring Side Effects : Keep track of any side effects you experience and communicate them to your healthcare team. They can offer advice and adjustments to manage them.
- Follow-Up Appointments : Your medical team will schedule regular follow-up appointments to monitor your progress, assess side effects, and make any necessary treatment adjustments.
- Gradual Recovery : Recovery is usually gradual. Over time, your body will recover from the effects of chemotherapy, and you'll start feeling more like yourself.
- Returning to Activities : As you start feeling better, you can gradually resume your daily activities and exercise routine. It's important to listen to your body and avoid pushing yourself too hard.
- Emotional Support : Give yourself permission to experience a range of emotions during recovery. Connecting with support groups, therapists, or counselors can be helpful.
Lifestyle changes after Chemotherapy procedure:
After undergoing chemotherapy, making certain lifestyle changes can support your recovery, enhance your well-being, and promote long-term health. Here are some lifestyle adjustments to consider:
- Prioritize Self-Care: Focus on self-care, including getting adequate rest, staying hydrated, and engaging in activities that bring you joy and relaxation.
- Balanced Nutrition: Opt for a balanced diet rich in fruits, vegetables, lean proteins, whole grains, and healthy fats. Proper nutrition can aid in your body's recovery and help manage side effects.
- Hydration: Drink enough water to stay hydrated. Proper hydration can alleviate some side effects and aid in the elimination of toxins from your body.
- Physical Activity: Engage in regular, gentle physical activity as your energy levels permit. Exercise can boost your mood, improve strength, and support overall well-being.
- Gradual Return to Routine: Ease back into your daily routine, taking into consideration your energy levels and physical capacity. Listen to your body and avoid overexertion.
- Mind-Body Practices: Consider incorporating relaxation techniques such as meditation, deep breathing, and yoga to manage stress and anxiety.
- Supportive Relationships: Surround yourself with supportive friends, family, or support groups. Emotional connections can contribute to your emotional well-being.
- Adequate Sleep: Prioritize sleep and establish a regular sleep schedule. Quality sleep aids in your body's healing process.
- Sun Protection: Protect your skin from the sun by using sunscreen, wearing protective clothing, and seeking shade. Some chemotherapy drugs can increase sensitivity to sunlight.
- Dental Care: Pay attention to oral hygiene and visit your dentist regularly. Chemotherapy can affect oral health, so it's important to maintain good dental care.
- Emotional Well-Being: Seek emotional support through therapy, counseling, or support groups if you're dealing with anxiety, depression, or other emotional challenges.
- Professional Guidance: Consult your healthcare team before making significant lifestyle changes to ensure they align with your recovery and treatment plan.
- Limit Alcohol and Tobacco: Reduce or eliminate alcohol consumption, as it can interact with medications and hinder recovery. If you smoke, consider quitting to improve your overall health.
- Manage Stress: Practice stress-management techniques such as mindfulness, hobbies, or spending time in nature to reduce stress levels.
- Stay Informed: Educate yourself about potential long-term effects of chemotherapy, and discuss any concerns with your healthcare team