Best Doctor for Celiac Disease Treatment and Get Right Treatment
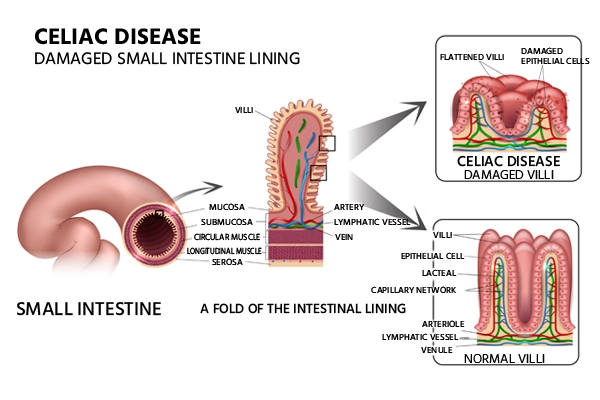
Celiac disease is an autoimmune disorder that is induced by gluten consumption. Celiac sprue, nontropical sprue, and gluten-sensitive enteropathy are the other names for this condition. When someone with celiac disease consumes gluten, their body reacts badly to the protein, causing damage to their villi, which are small finger-like projections along the wall of their small intestine.When the villi are damaged, the small intestine cannot absorb nutrients from food properly. This can eventually lead to malnourishment, bone density loss, miscarriage, infertility, neurological problems or certain cancers.
If the celiac disease does not improve after at least a year of no gluten, it is referred to as refractory or nonresponsive celiac disease. Most celiac disease patients are unaware of their condition. According to researchers, as few as 20% of people with the disease receive the correct diagnosis. Celiac illness is not the same as gluten intolerance or gluten sensitivity. Gluten intolerant people may experience some of the same symptoms and choose to avoid gluten. Now let us look at the types of Celiac Disease, their symptoms, causes, diagnosis and treatment for Celiac Disease.
If the celiac disease does not improve after at least a year of no gluten, it is referred to as refractory or nonresponsive celiac disease. Most celiac disease patients are unaware of their condition. According to researchers, as few as 20% of people with the disease receive the correct diagnosis. Celiac illness is not the same as gluten intolerance or gluten sensitivity. Gluten intolerant people may experience some of the same symptoms and choose to avoid gluten.
Types of Celiac Disease
There are different types of celiac disease:
- Classical celiac disease
- Non-classical celiac disease
- Silent celiac disease
- Potential celiac disease
- Refractory celiac disease
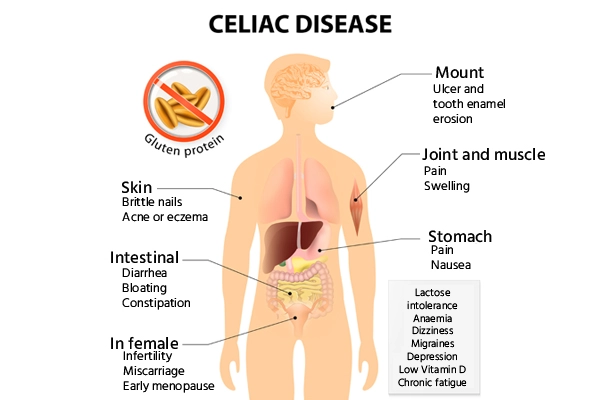
Symptoms of Celiac Disease
The celiac disease is not the same as a
food allergy,
so the symptoms are also different. If you are allergic to wheat but eat something containing wheat, you may experience itchy or watery eyes or difficulty breathing.
Celiac disease symptoms in adults
If you have celiac disease and accidentally consume gluten, you may have symptoms like:
Celiac disease symptoms in children
Celiac disease increases the chances of digestive issues in children.
Causes of Celiac Disease
Normally, the body's immune system is designed to protect it against foreign invaders. When people with celiac disease consume gluten-containing foods, their immune systems attack the intestine lining. This causes inflammation (swelling) in the intestines and damages the villi, hair-like structures on the small intestinal lining. The villi absorb nutrients from food. If the villi are injured, the patient cannot absorb nutrients and becomes malnourished, regardless of how much they consume.
Risk Factors of Celiac Disease
Celiac disease tends to be more common in people who have:
- A family member with celiac disease or dermatitis herpetiformis
- Diabetes type 1
- Turner syndrome or
Down syndrome
-
Thyroid
autoimmune disease
- Microscopic colitis (lymphocytic or collagenous colitis)
- Addison's syndrome
Complications
Untreated, celiac disease can cause:
-
Malnutrition: Malnutrition develops when your small intestine is unable to absorb adequate nutrients. Anaemia and weight loss can result from malnutrition. It can induce poor development and short stature in children.
-
Bone weakening:
Deficiency of calcium
and
vitamin D
can cause bone softening (osteomalacia or rickets) in children and bone density loss (osteopenia or
osteoporosis)
in adults.
-
Infertility and miscarriage: Malabsorption of calcium and vitamin D might contribute to infertility and miscarriage.
-
Lactose intolerance: Damage to the small intestine can cause stomach discomfort and diarrhea after eating or drinking lactose-containing dairy products. You may be able to accept dairy products again once the intestine has recovered.
-
Nervous system problems: Some celiac disease patients may experience seizures or nerve disorders in their hands and feet (peripheral neuropathy).
-
Cancer: People with celiac disease who do not follow a gluten-free diet are more likely to develop cancer, including intestinal lymphoma and small intestine cancer.
Diagnosis of Celiac Disease
A physical examination and a medical history are used to make a diagnosis. Doctors will also perform various tests to assist confirm a diagnosis. Antiendomysium (EMA) and anti-tissue transglutaminase (TGA) antibodies are frequently elevated in celiac disease patients. Blood testing can detect these conditions. They are the most reliable when tests are conducted when gluten is still present in the diet.
Common blood tests include:
A skin biopsy can help doctors detect celiac disease in persons with dermatitis. The doctor will extract microscopic bits of skin tissue for examination under a microscope during a skin biopsy. If the skin biopsy results and blood tests suggest celiac disease, an internal biopsy may not be required.
When blood tests or skin biopsies are inconclusive, an
upper endoscopy
can be used to diagnose celiac disease. During an upper endoscopy, a narrow tube called an endoscope is put through the mouth and down into the small intestines. The doctor can inspect the intestines and check for villi damage using a tiny camera linked to the endoscope. In addition, the doctor can do an intestinal biopsy, which includes removing a tissue sample from the intestines for analysis.
Treatment for Celiac Disease
The only way to treat celiac disease is to eliminate gluten from the diet. This permits the intestinal villi to recover and begin correctly absorbing nutrients. The doctor will instruct patients on how to eliminate gluten while eating a good and healthy diet. They will also educate you on how to read food and product labels so you can detect any gluten-containing ingredients.
When gluten is removed from the diet, symptoms might improve within days. However, patients should not stop consuming gluten until they have been diagnosed. Premature gluten removal may interfere with test findings and result in an incorrect diagnosis.