- Cardiology 84
- Dermatology 45
- Endocrinology 33
- ENT 16
- Fertility 190
- Gastroenterology 78
- General-Medicine 81
- Gynecology 80
- Hematology 19
- Infectious-Diseases 33
- Neurology 52
- Oncology 34
- Ophthalmology 23
- Orthopedics 69
- Pediatrics 31
- Procedure 23
- Public-Health 144
- Pulmonology 59
- Radiology 8
- Urology 68
- Wellness 161
- Woman-and-child 77

What is ECMO?
Extracorporeal membrane oxygenation (ECMO) is a treatment that temporarily replaces the functioning of the heart and lungs in critical conditions.
ECMO temporarily takes over the work of the heart and lungs, so they can heal from an emergency or critical situations like heart or lung failure.
ECMO is a life-saving procedure that helps the heart and lungs to heal, but it's not a cure for lung and heart diseases.
EIt works by extracting blood from the patient and pumping that blood through an artificial lung, exchanging oxygen and carbon dioxide, then sending the blood back to the patient via a pump that takes over the work of the heart.
Get a second opinion from trusted experts and makeconfident, informed decisions.
Get Second OpinionWhy is ECMO used?
ECMO can be used in any age group, from infants to adults who are in critical conditions of the heart, lungs, or who are recovering from heart transplantation.
Some heart conditions which ECMO can be used include:
- Life-threatening response to infection
- Birth defects of the heart
- Low body temperature
- Myocarditis
- Post-transplant complications
- Acute myocardial infarction
- Heart muscle disease
- cardiogenic shock
Some heart conditions which ECMO can be used include:
- Congenital diaphragmatic hernia or Defect in the diaphragm
- Blockage in a pulmonary artery in the lungs
- Acute respiratory distress syndrome
- Meconium aspiration syndrome (MAS)
- Extreme high blood pressure in the arteries of the lungs (PPHN)
How does ECMO Machine work?
- The ECMO machine is connected to a patient through plastic tubes called a cannula into large veins and arteries in the leg, neck, or chest.
- ECMO Machine works by removing blood from the patient and pumping that blood through an artificial lung, replacing oxygen and carbon dioxide, then sending the blood back to the patient via a pump that takes over the functioning of the heart.
Your health is everything - prioritize your well-being today.
Schedule Your AppointmentWhat are the different modes of ECMO?
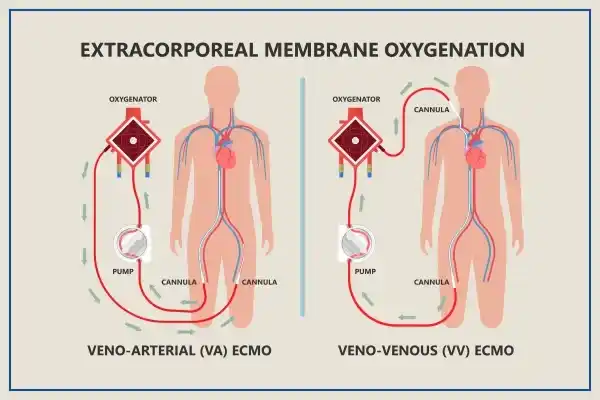
ECMO is used in two different ways depending on the patient’s requirement:
Veno-Arterial ECMO(VA - ECMO)
- Veno-Arterial ECMO (VA ECMO) is one type that supports both lung and heart function. Two cannulas are placed one in a large vein and the other in a large artery, on the side of the neck, directly into the chest or in the leg.
- The ECMO machine will take the blood out of the vein, add the oxygen and remove the carbon dioxide, and then return the blood to the artery and pump the blood through the body.
Veno-venous ECMO (VV- ECMO)
- Veno-Venous ECMO (VV ECMO) is another type that only supports lung function. One or two cannulas are placed in large veins on the side of the neck or in the leg.
- Whether to place one or two cannulas depends on the condition of the patient. It pumps blood through the heart to arteries that carry the oxygenated blood to organs and other body tissues, so that the lungs get enough rest and recover soon.
Ecmo Treatment
Monitoring patients during ECMO
- Patients who are on the ECMO will be on continuous observation to measure their heart rate, blood pressure, and oxygen levels.
- The blood is tested frequently to check the carbon dioxide and oxygen levels in the blood and to make sure the blood is thin enough.
- All these tests are done to make sure the ECMO machine is helping the patient’s health and to make changes if needed.
Preventing lung infections during ECMO
- Sometimes patients develop lung infection in mucus formation. With a tube called an endotracheal tube (ET tube), the mucus is sucked out of the lungs.
- This helps the lung free from mucus and infection.
Healing the lungs while on ECMO
When the patient is on the ECMO machine, it takes over the lung functioning temporarily and helps in healing the lungs.
Allowing action during ECMO
- Medication is given to the patients to reduce the pain and make them comfortable.
- These medicines may make them sleepy, while some patients are awake and able to talk and interact while on ECMO.
- Sometimes, patients are active and able to walk while on ECMO.
Nutrition during ECMO
- Nutrients provided to patients come from different sources including, central venous nutrition (CVN) and lipids (CVN supply required vitamins, electrolytes, and lipids supply fats) medication is given through a vein.
- For some patients who have Endotracheal Tube (ET tube), the nutrients are given in the liquid form directly into the stomach through a tube.
What is the risk of ECMO?
Though ECMO is a life-saving procedure, it can be associated with a few risks due to its complexity, which includes:
Bleeding
- A blood-thinning medication is needed for the patients while on ECMO, due to this they can start bleeding in different parts of their body (brain, lungs, insertion sites of the cannula).
- As bleeding can be very serious, the patient will be given certain medications to help the blood clot.
- In some cases, surgery is needed to stop the bleeding. Blood and blood platelets are given to the patient if the blood count drops.
Blood clot (thromboembolism)
- Sometimes blood clots or air bubbles appear inside the ECMO tubes. So, the healthcare team frequently monitors for preventing blood clots or air bubbles while the patient is on ECMO.
- A medicine called heparin helps the blood from clotting. This helps in reducing the chance of an air bubble reaching organs or a blood clot blocking a blood vessel, so that blood can reach an organ.
Infection
- The infection can develop from the sites where the tubes enter the body and can spread to the lungs, or the other body parts.
- If any signs of infection are identified, the patient will be given antibiotics.
Stroke
- When a patient is on ECMO, certain areas of the brain may not get as much blood flow as they need because of small blood clots, this can cause a stroke and some parts of the brain may be damaged permanently.
- The damaged part of the brain determines what problem a person may develop due to stroke. A stroke may restrict one's capability to move certain parts of their body, see, remember, speak, read, or write.
- Only a few people who were affected by the stroke may recover function after stroke. Strokes are very rare and happen to less than 5% of the people on ECMO.
Conclusion
ECMO is a complex yet life-saving procedure that potentially benefits patients in critical conditions.
However, the success rates of ECMO depend on the severity of the patient’s health condition that has led to the need for ECMO.
The doctor will explain to what extent the ECMO can be helpful according to the patient's condition.
Frequently Asked Questions
ECMO (Extracorporeal Membrane Oxygenation) is a life-support machine that takes over the function of the heart and lungs. It oxygenates the blood outside the body, allowing the heart and lungs to rest and heal.
No, ECMO is not done for every heart patient. It is typically used for patients with severe heart or lung conditions that do not respond to conventional treatments. ECMO is often considered a last resort.
During the ECMO process, complications such as bleeding, infection, and blood clots can occur. The decision to use ECMO is made based on the potential benefits and risks, and it is usually used in critical situations where the patient's condition is life-threatening.
Yes, ECMO can be used for children and infants with severe heart or lung conditions. Pediatric ECMO is similar to adult ECMO but requires specialized equipment and expertise.
A ventilator helps patients breathe by pushing air into the lungs, while ECMO oxygenates the blood outside the body and can provide support for both the heart and lungs.
ECMO can have side effects, including bleeding, blood clots, infections, and complications related to cannulation (insertion of tubes). The medical team takes measures to minimize these risks and manage any complications that arise.

- Cardiology
- Case Studies
- Dermatology
- Endocrinology
- ENT
- Fertility
- Gastroenterology
- General
- General-Medicine
- Gynecology
- Hematology
- Infectious-Diseases
- Medical News
- Neurology
- Oncology
- Ophthalmology
- Orthopedics
- Pediatrics
- Procedure
- Public-Health
- Pulmonology
- Radiology
- Second Opinion
- Urology
- Wellness
- Woman-and-child