Permanent pacemakers represent an important therapy for patients with severe bradyarrhythmia. Conventionally, ventricular pacing is performed by implanting the lead in the right ventricle (RV), at the apex or septum. This abnormally activates the ventricles, leads to desynchrony of contraction, and can cause left ventricular systolic dysfunction and heart failure in the long run. The newer technique of conduction system pacing (CSP) aims to use the heart’s native conduction system to deliver pacing so that the ventricles are activated in a manner that is closely similar to their usual pattern of activation.
This provides a physiologic form of pacing and yields better long-term outcomes compared to conventional RV pacing. CSP can be performed by either His bundle pacing or left bundle branch area pacing (LBBP) and requires specialized technique and skill on the part of the operator. In this article, two cases of LBBP carried out at Medicover Hospitals, Hitech City is described.
Case 1
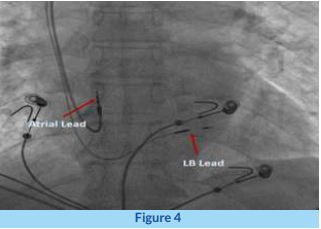
A 62-year-old female diabetic, hypertensive presented with dyspnoea on exertion, fatigue, and dizziness. ECG showed a complete heart block (CHB) with a narrow QRS escape rhythm (Figure 3A). An echocardiogram showed normal LV systolic function. 3A: ECG showing complete heart block with narrow QRS escape. 3B: ECG after left bundle branch pacing showing narrow paced QRS,almost identical to the original native QRS.
The patient was taken up for dual-chamber permanent pacemaker implantation to perform CSP. A quadripolar electrophysiology diagnostic catheter was placed from the femoral route in the His location to have a fluoroscopic landmark to guide the positioning of the ventricular lead. Using a Medtronic 3830 lead (Medtronic Parkway, Minneapolis, MN, USA) and a C315 His sheath (Medtronic limited, Croxley Park, Hatters Lane, Building 9, UK/Ireland). His Bundle pacing was first attempted; however, due to an abnormally high location of the His, satisfactory lead stability could not be obtained.
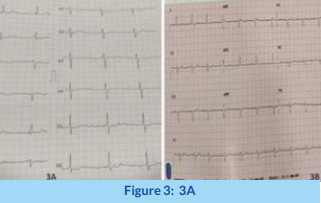
Hence, the strategy was switched to LBBP. Using the same sheath and lead, the correct location in the interventricular septum was reached, guided by the location of the His catheter and QRS morphology on pacing through the lead. Then, five to six rapid turns with the lead were given to penetrate the interventricular septum. Using careful analysis of multiple parameters such as QRS morphology, lead impedance, measurement of activation times, and mapping of potentials, additional turns were given to position the lead at the right depth in the IVS to achieve optimal LB capture.Excessive penetration risks perforation into the LV cavity. After confirming excellent LB capture parameters, the delivery sheath was slit, and lead secured.
The fluoroscopic location of the LB pacing lead is shown in Figure 4. The procedure was completed after placing the RA lead and pacemaker pulse generator. The post-procedure ECG with ventricular pacing from the LB lead is shown in Figure 3B. We can appreciate that the QRS is quite narrow (98 milliseconds) and almost similar to the native QRS in appearance. The patient had complete resolution of symptoms and was discharged uneventfully.Anteroposterior fluoroscopic view showing the positions of the right atrial (RA) and left bundle (LB) lead.
Case 2
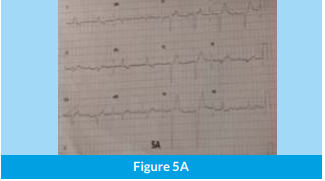
A 74-year-old male, diabetic and hypertensive, presented with significant shortness of breath for the past 4- 5 days, associated with dizziness. ECG revealed2:1 AV block with a very prolonged PR interval for the conducted beat and every alternate p wave blocked. Additionally, the QRS was broad, with a QRS duration of 150 milliseconds (ms), with a left bundle branch block (LBBB) morphology (Figure 5A). The patient a lso had intermittent complete heart block.
Echocardiography showed normal LV systolic function and coronary angiography showed minor coronary artery disease. After initial stabilization with a femoral temporary pacing wire, he was taken up for permanent pacemaker implantation with a dual- chamber pacemaker.
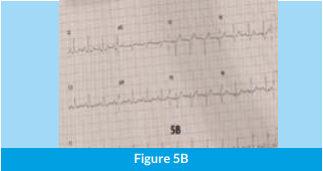
Because of potential infra-Hisian AV block, it was decided to perform LBBP straightaway rather than His bundle pacing. Using a similar approach as in Case 1, the pacing lead was screwed into the correct location in the IVS, and good LB capture parameters were obtained. The post- procedure ECG with ventricular pacing from the LB lead is shown in Figure 5B. A comparison of this ECG to the pre-procedure ECG demonstrates how the QRS has significantly narrowed to 95 ms, with complete correction of LBBB.
The patient had excellent recovery with complete relief of symptoms and was discharged on day 2. 5A: ECG showing complete heart block with broad QRS escape of left bundle branch block (LBBB) morphology. 5B: Post pacemaker ECG showing narrow-paced QRS, with complete correction of LBBB.
Discussion
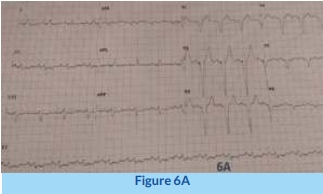
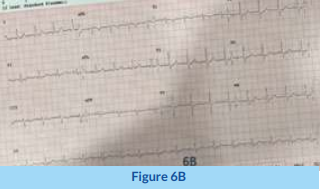
The above two cases demonstrate how CSP can be used to achieve very gratifying results in terms of QRS morphology and avoiding the risk of pacing cardiomyopathy. To better appreciate the difference from usual RV pacing, an ECG with regular RV pacing versus LBBP is shown in Figure 6. Contrasting conventional right ventricular (RV) pacing with broad QRS (6A), versus left bundle branch (LBB) pacing with narrow QRS (6B).
Additionally, as Case 2 demonstrates, pre-existing bundle branch block can be overcome using CSP; thus, it can be an excellent alternative to CRT in selected cases, yielding both better results and reducing the cost of the procedure considerably as CRT can be performed with just a dual-chamber pacemaker, rather than an expensive CRT device. However, in CRT candidates with pre- existing cardiomyopathy, the risk of diffuse conduction system disease is higher due to fibrosis, with subsequently a risk of failure to correct bundle branch block by CSP which shouldbe kept in mind.
The need for a concomitant defibrillator (ICD) will also determine the type of device chosen. Nevertheless, CSP is being performed in many cases as an alternative to CRT with good results. At our center, we have been performing CSP over the past 2 years and aim to gradually expand the numbers with the ultimate aim of making it the default approach to cardiac pacing. Ongoing studies with CSP and worldwide experience will give us more information and confidence in this regard.
Conclusion
The newer technique of conduction system pacing (CSP) aims to use the heart’s native conduction system to deliver pacing so that the ventricles are activated in a manner that is closely similar to their usual pattern of activation. This provides a physiologic form of pacing and yields better long-term outcomes compared to conventional RV pacing. CSP can be performed by either His bundle pacing or left bundle branch area pacing (LBBP) and requires specialized technique and skill on the part of the operator.
Contributors
Consultant Cardiologist & Electrophysiologist
News Letter
Medicover Hospitals Impact Newsletter August 2022