Best Treatment for Prostatectomy at an Affordable Price
Prostatectomy is a surgical procedure designed to
address various prostate-related conditions, most notably prostate cancer
and benign prostatic hyperplasia (BPH). This surgical intervention involves
the removal of all or a portion of the prostate gland, a walnut-sized organ
located below the bladder in males. Prostatectomy is considered a key
treatment option when non-surgical approaches prove inadequate or when the
condition poses significant health risks.
Steps involved in Prostatectomy Procedure
Prostatectomy surgery involves the removal of all or part of the
prostate gland, a male reproductive organ located beneath the bladder and surrounding
the urethra. This surgical procedure is commonly performed to treat conditions such as
prostate cancer and benign prostatic hyperplasia (BPH). The specific steps of a
prostatectomy surgery can vary depending on the approach used, but here is a general
overview of what typically happens during the procedure:
- Preparation: Before the surgery, the patient will undergo a
thorough medical evaluation and may need to undergo various tests to
assess their overall health and the extent of the prostate condition.
This information helps the surgical team plan the procedure.
- Anesthesia: Prostatectomy is usually performed under general
anesthesia, which means the patient is asleep and pain-free during the
surgery.
- Incision: The surgeon makes an incision in the patient's lower
abdomen or between the anus and scrotum, depending on the chosen
approach. The size and location of the incision depend on the type of
prostatectomy being performed.
- Access to the Prostate: The surgeon carefully moves aside tissues
and organs to gain access to the prostate gland.
- Prostate Removal: The surgeon then removes the prostate gland,
along with any surrounding tissue or lymph nodes if necessary. The
extent of removal depends on the reason for the surgery.
- Closure: After the prostate is removed, the surgeon sutures or
staples the incision closed.
- Drainage and Catheter: A thin tube (drain) may be placed near the
incision to help drain any excess fluids that might accumulate.
Additionally, a urinary catheter is usually inserted through the penis
into the bladder to allow urine to drain while the surgical site heals.
- Recovery and Observation: After the surgery, the patient is
monitored closely in a recovery area as they wake up from anesthesia.
The drainage tube and urinary catheter remain in place for a certain
period, typically a few days.
- Hospital Stay: The length of the hospital stay can vary depending
on the type of prostatectomy performed and the patient's overall health.
Some procedures, such as robotic-assisted laparoscopic prostatectomy,
may result in a shorter hospital stay.
- Follow-Up Care: Once the patient is discharged, they will receive
detailed instructions for post-operative care, including managing the
catheter, caring for the incision, and monitoring for any signs of
complications.
Indications of Prostatectomy Surgery
Prostatectomy surgery is indicated for certain medical conditions
affecting the prostate gland. The decision to perform a prostatectomy is typically based
on the severity of the condition, the potential benefits of surgery, and the overall
health and preferences of the patient. Here are some common indications for
prostatectomy surgery:
- Prostate Cancer: Prostatectomy is a primary treatment option for
localized prostate cancer, where the cancer is confined to the prostate
gland and has not spread beyond. It may also be considered for more
advanced cases if the cancer is still confined to the prostate area.
- Benign Prostatic Hyperplasia (BPH): For men with severe symptoms
of BPH, such as urinary retention, frequent urinary tract infections,
kidney damage, or significant quality of life impact, prostatectomy may
be recommended to relieve urinary obstruction and improve urinary flow.
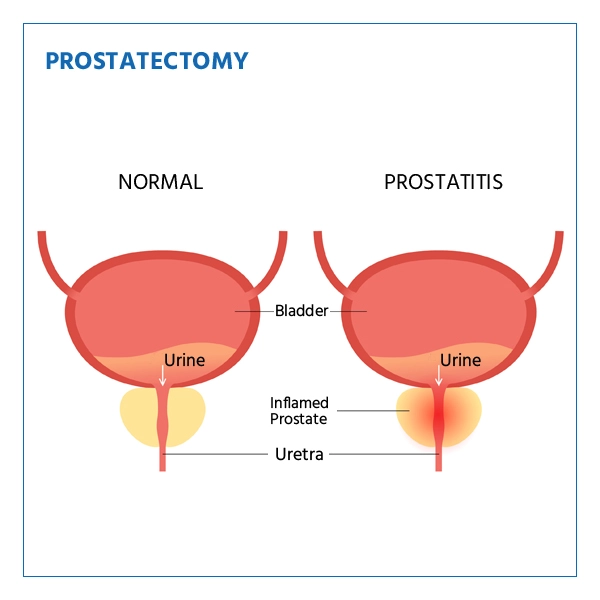
- Prostatitis: In cases of chronic prostatitis that do not respond
to other treatments and cause persistent pain and discomfort, a
prostatectomy may be considered as a last resort.
- Prostate Gland Enlargement: In some cases, when medications and
other non-surgical treatments fail to alleviate symptoms of an enlarged
prostate (BPH), a prostatectomy might be suggested.
- Prostate Abscess: A prostate abscess is a pus-filled cavity
within the prostate. If antibiotics and drainage procedures are
ineffective, surgery might be necessary.
- Recurrent Urinary Tract Infections: Chronic urinary tract
infections caused by prostate issues that are unresponsive to other
treatments may lead to consideration of a prostatectomy.
- Obstructive Uropathy: This condition involves blockage of the
urinary tract due to an enlarged prostate or other prostate-related
issues, leading to kidney damage. Prostatectomy may be indicated to
relieve the obstruction and restore kidney function.
Who will treat for Prostatectomy
Prostatectomy surgery is typically performed by a urologist, a
medical doctor who specializes in the diagnosis and treatment of conditions related to
the urinary tract and male reproductive system. Urologists are highly trained in
surgical techniques and procedures involving the prostate gland. They have the expertise
to assess your condition, recommend appropriate treatment options, and perform
prostatectomy surgery if necessary.
Here are the key steps involved in the process of prostatectomy
surgery:
- Discussion of Treatment Options: The urologist will go over your
treatment choices, including the potential advantages and disadvantages
of prostatectomy surgery, based on the findings of the evaluation. They
will also respond to any queries or worries you might have.
- Surgical Planning: If prostatectomy surgery is recommended, the
urologist will explain the specific type of prostatectomy that best
suits your condition. There are different approaches, including open
surgery, laparoscopic surgery, and robotic-assisted surgery. The
urologist will outline the procedure and discuss the expected outcomes.
- Surgery: The urologist will perform the prostatectomy surgery,
removing all or part of the prostate gland, as indicated by your
condition. The surgical technique and approach may vary depending on
factors such as the size of the prostate, the presence of cancer, and
your overall health.
- Recovery and Follow-Up: After the surgery, the urologist will
provide post-operative care instructions, monitor your recovery, and
schedule follow-up appointments to track your progress and address any
concerns.
Preparing for Prostatectomy Surgery
Preparing for prostatectomy surgery involves a combination of
physical and emotional preparations to ensure a successful procedure and smooth
recovery. Here's a comprehensive guide on how to prepare for prostatectomy surgery:
- Medical Evaluation and Consultation:
- Attend all pre-surgery appointments and consultations with your
urologist.
- Provide accurate information about your medical history, current
medications, allergies, and any previous surgeries.
- Undergo any necessary tests, such as blood work, imaging
studies, and prostate biopsies.
- Education and Information:
- Fully understand the procedure, including the type of
prostatectomy planned, potential risks, benefits, and expected
outcomes.
- Ask your urologist any questions you may have about the surgery,
recovery, and long-term effects.
- Lifestyle Adjustments:
- Follow any preoperative dietary restrictions or guidelines
provided by your healthcare team.
- Quit smoking and limit alcohol consumption, as these factors can
affect your healing and recovery.
- Medication Management:
- Inform your urologist about all medications you are taking,
including prescription, over-the-counter drugs, and supplements.
- Your urologist will provide instructions on which medications to
continue, stop, or adjust prior to surgery.
- Hygiene and Skin Preparation:
Shower using an antibacterial soap the night before or on the morning of
the surgery to reduce the risk of infection.
- Fasting:
Follow the fasting instructions provided by your healthcare team,
usually starting the night before the surgery. This helps prevent
complications during anesthesia.
- Arrangements for After Surgery:
- Arrange for a responsible adult to accompany you to the hospital
and drive you home after the surgery.
- Ensure you have a comfortable recovery space prepared at home,
including necessary supplies.
- Clothing and Personal Items:
- Wear loose, comfortable clothing on the day of surgery.
- Leave valuables at home, and only bring essential personal
items.
- Mental and Emotional Preparation:
- Practice relaxation techniques, such as deep breathing or
meditation, to help manage pre-surgery anxiety.
- Seek emotional support from friends, family, or support groups.
- Final Instructions:
- Follow any specific preoperative instructions provided by your
healthcare team regarding when to stop eating, drinking, or
taking medications.
- Arrive at the hospital on time for your scheduled surgery.
- Questions for Your Healthcare Team:
- Clarify any remaining doubts or concerns with your urologist
before the surgery.
- Ask about post-operative care, expected recovery time, and
potential complications.
Recovery After Prostatectomy Procedure
Recovery after prostatectomy surgery is a gradual process that
involves healing, regaining strength, and returning to your normal activities. The
specific timeline and experience can vary depending on the type of surgery, your overall
health, and how well you follow post-operative instructions. Here's an overview of what
to expect during the recovery period after prostatectomy surgery:
- Hospital Stay:
Most patients spend a few days in the hospital after prostatectomy
surgery, during which medical professionals monitor your condition,
manage pain, and ensure proper healing.
- Catheter Care:
A urinary catheter is typically placed during surgery to allow the
bladder to heal. Your healthcare team will teach you how to care for the
catheter and drainage bag.
- Physical Activity:
Start walking and moving around as soon as your healthcare team gives
you the green light. Gradually increase your activity level as you feel
comfortable, but avoid strenuous activities initially.
- Pain Management:
You may experience discomfort or pain around the incision site. Your
doctor will prescribe pain medication to help manage this during the
early stages of recovery.
- Incision Care:
Keep the incision site clean and dry as directed by your healthcare
team. Follow their instructions for changing dressings and caring for
the wound.
- Diet and Hydration:
Follow any dietary recommendations from your healthcare provider.
Staying hydrated and maintaining a balanced diet can aid in healing.
- Catheter Removal:
The urinary catheter is usually removed a week or two after surgery,
depending on your progress. Your healthcare team will guide you through
the removal process and provide instructions for managing urinary
function.
- Pelvic Floor Exercises:
Begin pelvic floor exercises (Kegel exercises) as advised by your
healthcare provider. These exercises can help improve urinary control
and support recovery.
- Follow-Up Appointments:
Attend all scheduled follow-up appointments with your urologist to
monitor your progress, discuss any concerns, and assess your healing.
- Return to Normal Activities:
As your recovery progresses, you'll be able to gradually resume normal
activities, including work, exercise, and social interactions.
- Sexual Function:
It's common for sexual function to be temporarily affected after
prostatectomy surgery. Discuss any concerns with your urologist, who can
provide guidance on managing and improving sexual function.
- Long-Term Follow-Up:
Even after your initial recovery, regular follow-up appointments will be
important to monitor your overall health and assess any potential
long-term effects of the surgery.
Lifestyle changes after Prostatectomy Procedure
After undergoing prostatectomy surgery, making certain lifestyle
changes can contribute to a smoother recovery, promote overall well-being, and support
your long-term health. Here are some important lifestyle adjustments to consider:
- Balanced Diet:
Consume a well-balanced diet rich in fruits, vegetables, whole grains,
lean proteins, and healthy fats. Adequate nutrition supports healing and
overall health.
- Hydration:
Drink plenty of water to stay hydrated. Proper hydration aids in
recovery and helps maintain urinary function.
- Physical Activity:
- Engage in light physical activity, such as walking, as advised
by your healthcare provider.
- Gradually increase your activity level as you regain strength
and stamina.
- Pelvic Floor Exercises:
Continue with pelvic floor exercises (Kegel exercises) to help improve
urinary control and strengthen the pelvic muscles.
- Avoid Heavy Lifting:
- Wait until your healthcare practitioner gives you the all-clear
before lifting anything heavy or doing anything difficult.
- until your healthcare provider gives you the go-ahead.
- Quit Smoking:
If you smoke, think about giving it up. Smoking might delay recovery and
raise the possibility of problems.
- Alcohol Moderation:
If you consume alcohol, do so in moderation. Limiting alcohol intake
supports your overall health and well-being.
- Medication Management:
Follow your doctor's instructions regarding medication use, including
pain relief and any prescribed medications.
- Sexual Activity:
Discuss resuming sexual activity with your urologist. They can provide
guidance on when it's safe to do so and how to manage any changes in
sexual function.
- Emotional Well-being:
It's important to get used to the physical and psychological changes
that follow surgery. If necessary, seek emotional assistance from close
friends, family members, or a mental health professional.
- Regular Follow-Up:
Keep up with all of your urologist's follow-up appointments to track
your recovery's progress and resolve any issues.
- Listen to Your Body:
Pay attention to your body's signals. Rest when you're fatigued and
avoid pushing yourself too hard too soon.
- Maintain a Healthy Weight:
Achieve and maintain a healthy weight through a combination of balanced
diet and appropriate exercise. This can support overall health and
well-being.
- Stay Informed:
Educate yourself about potential long-term effects of the surgery, such
as urinary changes, and learn strategies to manage them.
- Communicate with Your Healthcare Provider:
Stay in regular contact with your urologist. If you have questions or
concerns about your recovery or health, don't hesitate to reach out.