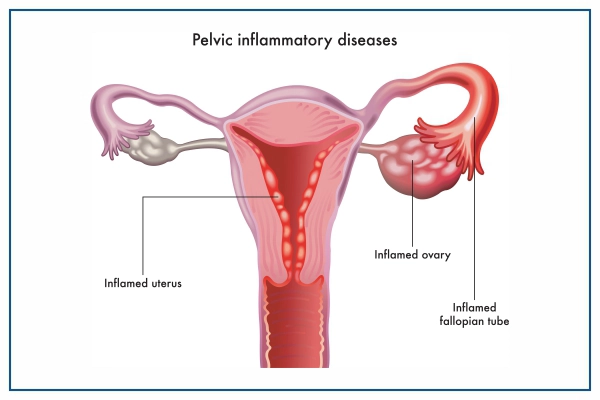
What is Pelvic Inflammatory Disease (PID)
PID is an infection affecting female reproductive organs, causing pelvic discomfort. Untreated, it can lead to ectopic pregnancy or chronic infection. Specific procedures like abortion can increase risk. PID progresses from the cervix to the fallopian tubes. Often symptomless, it's common in sexually active women aged 20-29.
What are the Symptoms of Pelvic Inflammatory Disease?
Some women with pelvic inflammatory disease may not show any symptoms. Women who do have symptoms may experience the following:
- Pain in the upper abdomen
- Painful sex
- Fever
- Painful urination
- Pain in the lower abdomen (the most common symptom)
- Irregular bleeding
- Tiredness
- Increased or foul-smelling vaginal discharge
Mild to severe discomfort can be caused by pelvic inflammatory disease. Some women, however, have significant discomfort and symptoms, such as
- Vomiting
- Sharp pain in the abdomen
- High fever (higher than 101°F)
- Fainting
When To See a Doctor?
Consult your doctor or seek emergency medical attention if you have any of the following symptoms:
- Foul smelling vaginal discharge
- Severe pain in the lower abdomen
- Fever, with a temperature higher than 101° F (38.3° C)
- Nausea and vomiting, with an inability to keep anything down
At Medicover, our team of Gynaecologists can help you deal with Pelvic Inflammatory Disease (PID) and its prevention.
What are the Causes of Pelvic Inflammatory Disease
Pelvic Inflammatory Disease (PID) is typically caused by a bacterial infection, most commonly transmitted through sexual activity. The primary bacteria responsible for PID are Chlamydia trachomatis and Neisseria gonorrhoeae, which are sexually transmitted infections (STIs). However, other bacteria can also cause PID, often when the normal balance of bacteria in the vagina is disrupted, allowing harmful bacteria to flourish.
Risk factors for PID include:
Those who have had gonorrhoea, chlamydia, or an STI, are more likely to develop pelvic inflammatory disease. However, PID can develop in the absence of an STI as well. Other factors that may increase the risk of PID include:
- Having sex when before the age of 25
- Having multiple sexual partners
- Having intercourse without the use of a condom
- Douching
- Recently having an intrauterine device (IUD) inserted
- Having a history of pelvic inflammatory disease
Complications of Pelvic Inflammatory Disease
- Infertility, or the inability to conceive a child.
- Ectopic pregnancy, wherein the fertilized egg fails to reach the uterus and implants itself in the fallopian tube, cervix or ovary.
- Chronic pelvic pain, which is linked to lower abdomen discomfort caused by inflammation of the fallopian tubes and other pelvic organs.
PID infection has the potential to spread to other places of the body. It may even be fatal if it spreads via blood.
Prevention of Pelvic Inflammatory Disease
- Reducing the number of sexual partners, and knowing their sexual history.
- Using a condom, before engaging in sexual activities.
- Testing oneself for STIs and HIV as having other STI’s or HIV increases the chances of contracting PID.
How to Diagnosis Pelvic Inflammatory Disease
After examining the patient’s medical history, as well as conducting a physical and pelvic examination, doctors decide on the best suited course of action. Other tests that may be performed are:
- A microscopic examination of vaginal and cervix samples
- Blood tests
- Pap test: For this test, cells from the cervix are removed and examined under a microscope. It can detect cancer, infection, or inflammation.
- Ultrasound: This test creates a picture of the organs using high-frequency sound waves.
- Laparoscopy: A small procedure performed with a laparoscope. It is a narrow tube with a lens and a light which is used to observe the reproductive tract through an incision in the abdomen wall.
- Culdocentesis: A needle is inserted into the pelvic cavity via the vaginal wall to get a sample of the pus.
Pelvic Inflammatory Disease of Treatment
Pelvic inflammatory illness is treatable, especially if detected early. Antibiotics are usually found to be effective in the treatment. Even if the symptoms go away, it's important to take all the medications exactly as the doctor prescribes. If one does not complete the medication course, symptoms may intensify. After starting the medication, the doctor may want to examine the patient again in a few days to check its progress.
The sooner one gets PID addressed, the better it is for their overall health. If PID is left untreated, it can cause serious damage and complications may occur.
If one has severe PID, hospitalisation may be advised. It may also be required if the patient is pregnant, under the age of 18, or has HIV.
Pelvic Inflammatory Disease Care at Medicover Hospitals
At Medicover, we have the best team of Gynaecologists and infectious disease specialists who work together to deliver the most comprehensive treatment for Pelvic Inflammatory Disease. Our highly qualified team utilises the latest medical approaches, diagnostic methods, and technologies to treat various gynaecological issues and ailments. We use a holistic approach to manage Pelvic Inflammatory Disease (PID) and provide personalised treatment to all our patients for a sustainable recovery.
