Advanced Treatment For Barrett's esophagus With Our Doctors
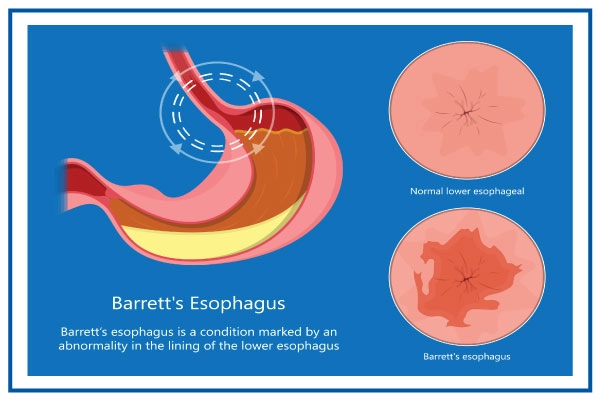
Barrett's esophagus (BE) is a condition in which the flat pink lining of the esophagus changes and becomes more like the lining of the small intestine rather than the esophagus.
The primary reason for Barrett’s esophagus is because of chronic inflammation resulting from Gastroesophageal Reflux Disease (GERD).
Gastroesophageal reflux disease (GERD) happens when stomach acid regularly moves back into the hollow muscular tube known as esophagus. This back flow of acid reflux can irritate the lining of the esophagus. GERD frequently comes with symptoms like regurgitation or heartburn. Barrett's esophagus may develop in a few people as a result of this GERD that changes the cells lining the lower esophagus.
A higher risk of esophageal cancer is linked to Barrett's esophagus. Even though there is a low chance of developing esophageal cancer, it is crucial to undergo routine health examinations with thorough imaging and extensive esophageal biopsies to look for precancerous cells (dysplasia). To prevent esophageal cancer, it is important to treat precancerous cells on time.
Symptoms
Barrett's esophagus does not have symptoms. Its symptoms are related to complications of chronic GERD, they are as follows:
- Frequent heartburn and stomach contents coming back up
- Having trouble swallowing food
- Occasionally, chest pain
- Black or bloody stools
- Vomiting blood
Only some patients with Barrett's esophagus report having significant acid reflux symptoms. As a result, you should talk to your doctor about your digestive health and the potential for Barrett's esophagus.
When to visit a doctor?
If you've experienced heartburn, regurgitation, or acid reflux for more than five years visit a doctor if you have-
- Chest pain that could be a sign of a heart attack
- Having trouble swallowing
- Vomiting crimson blood or coffee-ground-like blood
- Passing sticky, red, or black stools
Causes
The exact cause is unknown but it is mostly caused when the patients have GERD for a long time, many others do not have any symptoms of reflux, a condition known as "silent reflux."
It’s believed that the esophagus cells become abnormal with chronic exposure to stomach acid. Without GERD, Barrett's esophagus can develop, but patients with GERD are more vulnerable to develop Barrett’s esophagus.
Whether or not GERD symptoms coexist with acid reflux, chemicals and gastric acid wash back into the esophagus, eroding the tissues and producing changes to the lining of the swallowing tube that lead to Barrett's esophagus.
Risk factors
The following elements raise your risk of developing Barrett's esophagus:
Family background
If you have a family history of Barrett's esophagus or esophageal cancer, your chances of developing the condition increase.
Males
Barrett's esophagus is far more common in men.
Age
Although it can happen at any age, persons over 50 are more likely to develop Barrett's esophagus.
Acid reflux and persistent heartburn
Proton pump inhibitor use for GERD that doesn't improve or GERD that necessitates ongoing therapy can both raise the risk of Barrett's esophagus.
Smoking
People who do rigorous smoking are at more risk of this disease.
Overweight
Your risk is further increased by abdominal obesity.
Complications
Those who have Barrett's esophagus are more likely to get esophageal cancer. Even in patients whose esophageal cells have undergone precancerous alterations, the danger is minimal. Fortunately, esophageal cancer seldom occurs in patients with Barrett's esophagus.
Diagnosis
The most common method for diagnosing Barrett's esophagus is endoscopy. Your throat is examined with an endoscope, a lit tube with a camera at the end, to look for any indications of abnormal esophageal tissue. Normal esophageal tissue has a light, shiny appearance. The tissue of Barrett's esophagus is velvety and crimson.
Your esophagus will be biopsied by your doctor. To assess the level of change, the biopsied tissue is analysed.
Evaluating the extent of tissue alterations
The level of dysplasia in the cells of your esophagus is determined by a pathologist, a medical professional who specialises in studying tissue in a lab. The best way to confirm the diagnosis of dysplasia in the esophagus is to have it confirmed by two pathologists, at least one of whom should be an expert in gastrointestinal pathology.
Barrett's esophagus screening
Screening may be advised for males who have at least weekly GERD symptoms that don't improve with proton pump inhibitor therapy and who also have two or more additional risk factors, such as:
- Family history of esophageal cancer or Barrett's esophagus
- Males
- Having a 50+ age
- Smoking
- Belly fat
Treatment
The severity of the abnormal cell growth in the esophagus and your general health will determine the treatment procedure for Barrett's esophagus.
Zero or no dysplasia
Your doctor will probably advise:
- Regular endoscopy to check on the health of your esophagus's cells. You'll likely undergo a follow-up endoscopy in a year if your biopsies reveal no dysplasia, and then every three to five years if no alterations take place.
- Therapy for GERD: Your signs and symptoms may be lessened by medication and lifestyle modifications. To fix a hiatal hernia or to tighten the lower esophageal sphincter that regulates the flow of stomach acid, surgery or endoscopic techniques may be an alternative.
Minimal dysplasia or low-grade dysplasia
The earliest stage of precancerous alterations is thought to be low-grade dysplasia. If low-grade dysplasia is discovered, a skilled pathologist will confirm it. The doctor could advise having another endoscopy in six months for low-grade dysplasia and then having follow-up exams every six to 12 months after that.
However, if the diagnosis is confirmed, treatment might be advised given the danger of esophageal cancer. The preferred therapies consist of:
- Endoscopic resection helps identify dysplasia and cancer by removing damaged cells with an endoscope.
- Using heat, radiofrequency ablation removes aberrant esophageal tissue. After endoscopic resection, radiofrequency ablation might be advised.
- Cryotherapy involves applying a cold liquid or gas to aberrant esophageal cells using an endoscope. After allowing the cells to warm up, they are once more frozen. The aberrant cells are harmed by the freezing and thawing cycle.
High-grade dysplasia
The widespread consensus is that esophageal cancer is a precursor to high-grade dysplasia. For this reason, your doctor might suggest cryotherapy, radiofrequency ablation, or endoscopic excision. A surgical procedure in which the damaged segment of your esophagus is removed and the remaining portion is joined to your stomach, may also be a possibility.
Following treatment, Barrett's esophagus may return. Find out from your doctor how frequently you need to return for additional tests. Your doctor will probably advise lifelong medication to reduce acid and aid in the healing of your esophagus if you receive treatment other than surgery to remove aberrant esophageal tissue.
Lifestyle and self-care
Changes in lifestyle may help with GERD symptoms, which may be the cause of Barrett's esophagus. Consider the following precautions:
- Maintain a healthy weight.
- Avoiding foods and beverages including chocolate, coffee, wine, and mint that make you experience heartburn.
- Giving up smoking.
- Drink water
- Taking proper rest and sleep.
Do’s and Don’ts
In Barrett's esophagus the cells lining the esophagus appear similar to cells of the intestine. It occurs due to repeated exposure to stomach acid. A person with Barrett's esophagus has to follow sets of do’s and don’ts to manage it and its related complications.
| Do’s | Don’ts |
| Go for an endoscopy when you have GERD for a long time. | Leave GERD untreated. |
| Follow a healthy lifestyle. | Ignore when you vomit blood. |
| Visit the doctor when you have difficulty swallowing. | Do smoking or take alcohol. |
| Take proper rest and sleep. | Forget to take medications. |
| Maintain healthy body weight. | Lie flat straight at night. |
Barrett's esophagus symptoms include chest pain, difficulty swallowing, vomiting blood and bloody stools. Follow the above tips to prevent the condition or to lessen its symptoms.
Barrett's Esophagus Care at Medicover
At Medicover Hospitals, we have the most trusted team of doctors and paramedical staff who are experienced in providing excellent healthcare services to patients with compassion and care. Our diagnostic department is equipped with modern technology and equipment to conduct the tests required for the diagnosis of Barrett's esophagus based on which a dedicated treatment plan is designed. We have an excellent team of gastroenterologists who diagnose and treat this condition with utmost precision that brings successful treatment outcomes.