What is Atopic Eczema (Dermatitis)?
Written by Medicover Team and Medically Reviewed by Dr Anusha Nagral Reddy , Dermatologist
A common skin disorder characterized by itchy and inflamed skin patches is eczema, also known as atopic dermatitis or atopic eczema. It often appears on infants' faces but can affect children, teenagers, and adults in various ways. This chronic condition can flare up periodically and may be associated with asthma or hay fever, and make the skin red and itchy, which is atopic dermatitis (eczema). In children, it is normal, but it can occur at any age.
There is no cure for atopic dermatitis, but treatments and self-care can relieve itching and prevent new outbreaks. Key steps include avoiding harsh soaps, regularly moisturizing the skin, and using medicated creams or ointments.
Types of Atopic Dermatitis (Eczema)
The people usually mean atopic dermatitis, which they characterize as dry, itchy skin that often appears with a red rash. This is the most common and chronic type of eczema.
- Contact Dermatitis: Contact dermatitis is induced by irritant contact. It induces burning, scratching, and redness. When the irritant is removed, the inflammation goes away.
- Dyshidrotic Dermatitis: The fingers, hands, and soles of the feet are affected by dyshidrotic dermatitis. It causes itchy, scaly patches of flaking or red, broken, and painful skin. In women, the disorder is more common.
- Nummular Dermatitis: In the winter months, nummular dermatitis causes dry, round patches of skin. The legs are commonly affected by it. In men, it's more popular.
Atopic Dermatitis (Eczema) Causes
Eczema is a complex skin condition with multiple potential causes. It is thought to arise from a combination of genetic, environmental, and immune system factors. Here are some of the key factors and triggers that can contribute to the development or exacerbation of eczema:
- Genetics: Family history plays a significant role in the development of eczema. If you have close relatives with eczema, asthma, or allergic rhinitis (hay fever), you may be at a higher risk.
- Immune System Dysfunction: Eczema is often associated with an overactive immune response. In individuals with eczema, the immune system may react excessively to irritants or allergens, leading to skin inflammation.
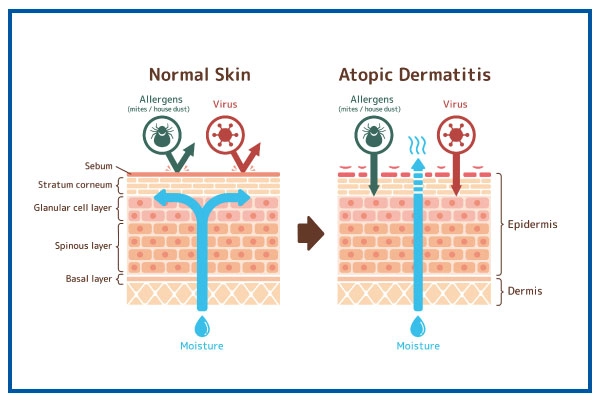
- Skin Barrier Dysfunction: The skin's outermost layer, called the epidermis, acts as a barrier that keeps moisture in and irritants out. In people with eczema, this barrier is compromised, allowing irritants, allergens, and bacteria to penetrate the skin more easily, leading to inflammation.
- Allergens: Allergens, such as pollen, dust mites, pet dander, and certain foods, can trigger or exacerbate eczema symptoms in some individuals, particularly those with allergic sensitivities.
- Irritants: Substances that can irritate the skin, such as harsh soaps, detergents, fragrances, and certain fabrics, can lead to eczema flare-ups.
- Climate and Weather: Cold, dry weather can lead to skin dryness and worsen eczema symptoms. Similarly, excessive heat and sweating can also trigger flare-ups in some individuals.
- Hormonal Changes: Hormonal changes, such as those that occur during pregnancy or menstruation, can affect eczema symptoms in some individuals.
- Microbial Infections: Bacterial, viral, or fungal infections can sometimes worsen eczema. Staphylococcus aureus, a type of bacteria, is known to colonize the skin of many people with eczema and can lead to skin infections.
Get a second opinion from trusted experts and makeconfident, informed decisions.
Get Second OpinionAtopic Dermatitis Symptoms
The atopic dermatitis symptoms vary depending on the age of the person. Eczema is more common in infants, and rubbing and scratching lead to skin infections. The symptoms in children and adults are different.
Symptoms in Infants
The following eczema symptoms are most common in infants under the age of 2
- Rashes on the skin
- Bubble-up rashes before fluid leaking
- Rashes that cause extreme itchiness and interfere with sleeping
Symptoms in Children
The following eczema symptoms are most common in children aged two and above
- Rashes that appear behind the elbows or the creases of the knees
- Rashes that occur between the buttocks and legs on the front, wrists, feet, and the crease
- Bumpy rashes
- Skin thickening
Symptoms in Adults
The Following are the symptoms that are common in adults
- Skin Infections
- Dry skin on the affected area
- Rashes on the body
- Rashes on the elbows and knees
Complications of Atopic Dermatitis (Eczema)
- Asthma and Hay Fever: These symptoms are also followed by eczema. Asthma and hay fever occur in more than half of young children with atopic dermatitis by the age of 13
- Chronic Itchy, Scaly Skin: With a patch of itchy skin, a skin disorder called neurodermatitis begins. You are scratching the place, which makes it even itchier. Eventually, purely out of habit, you can itch. The affected skin can become discolored, thick, and leathery because of this condition.
- Skin Infections: Open sores and cracks may be caused by frequent scratching that damages the skin. These raise the risk of bacteria and viruses, including the herpes simplex virus, causing infection.
- Irritant Hand Dermatitis: This particularly affects individuals whose work requires their hands to be wet and exposed to harsh soaps, detergents, and disinfectants.
- Allergic Contact Dermatitis: This is the most common in people with atopic dermatitis.
- Sleep Problems: The itch and scratch cycle can cause poor sleep quality.
Eczema Prevention
- Moisturize skin twice a day
- Identify and avoid triggers
- Shorter baths or showers
- Bleach bath
- Using gentle soaps
- Dry the skin soft towel and apply moisturizer
Foods To Eat (Atopic Dermatitis Self Care)
Eating such foods can cause the body to release immune system compounds that cause inflammation in people with eczema, which in turn leads to an eczema flare-up. A diet for anti-eczema is equivalent to an anti-inflammatory diet. Anti-inflammatory foods may include:
Fish
A natural source of fatty acids containing omega-3 that can combat inflammation in the body. Salmon, Albacore tuna, mackerel, sardines, and herring are examples of fish rich in omega-3s.
Foods High In Probiotics
Bacteria encourage the good health of the gut. Yogurt with living and active communities, miso soup, and tempeh are examples. Probiotics are also present in other fermented foods and beverages, such as kombucha, and sauerkraut.
Foods High In Inflammation-Fighting Flavonoids
It includes fruits and vegetables such as apples, broccoli, cherries, spinach, and kale.
Foods To Avoid
- Citrus Fruits
- Eggs
- Tomatoes
- Wheat
- Dairy products
- Soy
Diagnosis of Atopic Dermatitis (Eczema)
- Medical History: The healthcare provider will take a detailed medical history, including information about your symptoms, family history of eczema or allergies, and any potential triggers or exacerbating factors.
- Physical Examination: A thorough physical examination of your skin will be conducted to assess the appearance and distribution of the rash or affected areas.
- Skin Biopsy: In some cases, a skin biopsy may be performed to rule out other skin conditions that may mimic eczema.
Atopic Dermatitis (Eczema) Treatment Options
Frequently, eczema comes and goes. You may need to try various medications and other remedies to get rid of the rash when it occurs.
- Emollients (Moisturizers): Regularly applying emollient creams or ointments helps keep the skin hydrated and strengthens the skin barrier. This is a fundamental part of eczema management and helps reduce dryness and itching.
- Topical Corticosteroids: These anti-inflammatory creams or ointments are prescribed to reduce inflammation and itching during eczema flare-ups. They come in different strengths, and the choice of strength depends on the severity of the condition.
- Topical Calcineurin Inhibitors: Medications like tacrolimus and pimecrolimus are used topically to reduce inflammation and itching, especially in sensitive areas where corticosteroids may not be suitable.
- Antihistamines: Oral antihistamines can help relieve itching and improve sleep when itching is a significant symptom. They are often used in addition to other treatments.
- Wet Wrap Therapy: In severe cases or during acute flare-ups, wet wrap therapy involves applying a moisturizer and then damp dressings to the skin. This can help soothe and hydrate the skin.
- Avoidance of Triggers: Identifying and avoiding triggers like allergens, irritants, and certain foods can be an important part of eczema management. This can help prevent flare-ups and reduce the need for medication.
When to see a doctor?
One should immediately consult a physician in the following cases:
- Sleep disturbances and discomfort in performing day-to-day activities
- Infection on the skin, red streaks, pus, and/or yellow scabs
- Despite using home treatments, the skin issue persists
- Episodes of skin rash are followed by fever
Get the atopic dermatitis treatment from Top Dermatologists at Medicover Hospitals.
Your health is everything - prioritize your well-being today.
Risk Factors of Atopic Dermatitis (Eczema)
- Family History: A family history of eczema, asthma, or allergic rhinitis increases the risk of developing eczema.
- Age: Eczema often begins in childhood, with infants and young children being more susceptible. However, it can persist or develop at any age.
- Allergies: Allergic sensitivities to pollen, dust mites, pet dander, and certain foods can heighten the risk of eczema.
- Environmental Factors: Living in dry or cold climates can increase the likelihood of eczema, as can exposure to irritants and harsh weather conditions.
- Gender: Eczema is more common in females than males.
- Stress: High levels of stress or psychological factors can exacerbate eczema symptoms.
- Skin Type: Individuals with dry skin are more prone to developing eczema due to their skin's reduced barrier function.
- Occupational Exposures:Some professions that involve frequent exposure to irritants, chemicals, or allergens may increase the risk of developing occupational dermatitis, a type of eczema specific to workplace exposures.
Dos and Don'ts
A person with Atopic dermatitis has to follow a set of dos and don'ts to manage it and related symptoms and infections.
| Do's | Don'ts |
|---|---|
|
Keep Skin Moisturized: Apply moisturizers (emollients) regularly to keep the skin well-hydrated. Moisturize immediately after bathing or showering to lock in moisture. |
Scratch: Avoid scratching or rubbing the affected skin, as it can worsen inflammation and lead to skin infections. Keep your nails short and consider wearing soft cotton gloves at night to prevent scratching. |
|
Use Mild, Fragrance-Free Products: Choose mild, fragrance-free soaps, detergents, and skincare products to avoid irritating the skin. Look for products labelled as "hypoallergenic." |
Use Harsh Soaps: Avoid harsh soaps, perfumed body washes, and bubble baths, as they can strip the skin of natural oils and exacerbate eczema symptoms. |
|
Maintain Good Hygiene: Practice good hygiene by taking short, lukewarm baths or showers using mild cleansers. Pat your skin dry gently with a soft towel; avoid rubbing. |
Take Hot Showers or Baths: Hot water can dry out the skin and worsen eczema. Instead, use lukewarm water for bathing and showering. |
|
Identify and Avoid Triggers: Determine and avoid potential triggers that worsen your eczema symptoms. This may include specific foods, allergens, irritants, or environmental factors. |
Overuse of Corticosteroids: While topical corticosteroids can be effective for managing eczema, avoid overusing them. Follow your healthcare provider's instructions regarding their application, and do not use stronger corticosteroids on sensitive areas without guidance. |
|
Wear Soft, Breathable Fabrics: Opt for loose-fitting, soft, and breathable clothing made of natural fibres like cotton. Avoid rough, scratchy materials like wool. |
Skip Moisturizing: Consistently apply moisturizers even when your skin appears to be in good condition. Regular moisturizing helps prevent flare-ups. |
|
Seek Medical Advice: Consult a healthcare provider, preferably a dermatologist, for a proper diagnosis and personalized treatment plan. Follow your prescribed treatment regimen and attend follow-up appointments as recommended. |
Ignore Signs of Infection: If you notice signs of infection, such as increased redness, swelling, pain, or oozing from the affected skin, seek medical attention promptly. Skin infections can worsen eczema and require treatment with antibiotics or antiviral medications. |
Our Experience Treating Atopic Dermatitis (Eczema)
At Medicover Hospitals, we have the most trusted team of atopic dermatitis specialists, doctors, and medical experts experienced in providing empathetic healthcare services. Our diagnostic department is equipped with modern technology and equipment to conduct the necessary tests for diagnosing eczema. With an excellent team of dermatologists, we ensure precise diagnosis and treatment, delivering successful outcomes for patients.
