What is Knee Revision Surgery?
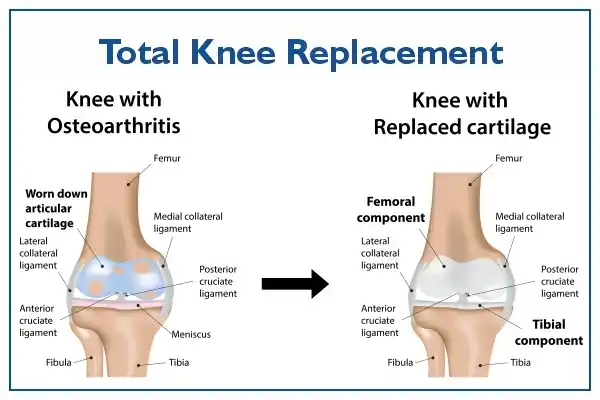
A knee revision is the replacement of prosthetic implants in a person who has previously had a complete knee replacement. In this surgery, known as "reoperation," an original prosthesis is removed and a new one is inserted. Some knee revisions may require the replacement of a single implant, while others require a complete exchange of all prostheses that were implanted during the original knee replacement surgery (known as "revision total knee replacement"). Such a complete revision is a complex procedure that requires extensive preoperative planning, specialized implants and tools, long surgical times, and mastery of difficult surgical techniques.
What is Failed Knee Replacement?
Most patients who undergo knee replacement surgery experience successful results, with lasting improvements in knee pain, mobility, and function. However, complications can occasionally arise after a knee replacement for various reasons, resulting in what is commonly known as a "failed knee replacement." When a knee replacement fails, either shortly after surgery or many years later, it may require a revision or "redo" of the knee replacement surgery.
Symptoms
Symptoms of a failed knee replacement can include:
- Pain, which can occur during activity or at rest.
- Swelling around the joint or recurring joint effusions
- Feeling like your knee wants to "give in" when standing, walking, or going up and down stairs downstairs
- Noticeable heat in the joint, long after the surgery is completed.
- Painful clicking or scratching noises
- A reduced range of motion and function.
- Inability to put weight on the leg.
If you experience any of these symptoms or other symptoms that concern you, it is important to have your surgeon evaluate you.
Causes
Wear and Loosening
The implants that work correctly depend on their adequate fixation on the bone. Fixation is generally achieved by cementing the implant to the bone. Some surgeons prefer to use biological fixation, which means that no cement is placed between the implant and the bone. Although implants are firmly fixed in the initial knee replacement surgery, they can loosen over time. The cause of loosening may not always be clear, but high-impact activities, excessive body weight, and wear on the polyethylene component can all act as contributing factors. The friction caused by the joint surfaces rubbing against each other wears down the implant surfaces, creating small particles that accumulate around the joint. The body's attempt to digest these wear particles destroys the implant's connection to the bone in a process known as aseptic loosening (not infected). During this process, normal, healthy bone is also digested (a condition called osteolysis), which can weaken or even fracture the bone. When the prosthesis becomes loose, the patient may experience pain, alignment changes, or instability.
Infection
With current surgical techniques and antibiotic regimens, the risk of infection from a total knee replacement is less than 1%. However, when it does occur, infection is a devastating complication of any surgical procedure. In a total knee replacement, large metal and plastic implants can serve as a surface for bacteria to adhere to, a process known as biofilm formation. The location of these bacteria makes them inaccessible to antibiotics. Even if the implants remain securely attached, revision surgery is necessary to stop the pain, swelling, and drainage of the infection.
Revision surgery for the infected knee can take several forms. Depending on the degree of infection and damage, the surgeon will determine one of two basic courses of action:
- Perform a simple knee wash while keeping the original prosthetic components in place
- Replace the implants completely with new ones in a complete revision operation of the knee.
A full infection check will involve a one or two-stage operation, depending on the severity of the infection and the virulence of the bacteria. In the single-stage operation, the previously infected components are removed as part of a full debridement, the knee is thoroughly cleaned, and the new revision components are placed in a surgical setting (i.e., same day). In the two-stage operation, two separate operations are performed weeks apart: the first operation is to remove the old prosthesis and insert a cement block with antibiotics (known as an antibiotic-impregnated cement spacer). The second surgery consists of removing the spacer and inserting a new prosthesis. Intravenous antibiotics are given frequently during both options to eradicate the infection.
Instability
Instability occurs when the soft tissue structures around the knee cannot provide the stability necessary for proper function when standing or walking. Increased soft tissue laxity (slack) or incorrect placement or alignment of the prosthesis can cause instability. The soft tissues, including the ligaments around the knee, may stretch after surgery and no longer provide the support that the knee needs. Pain and/or the feeling of the knee "giving in" can affect knee function. If these symptoms cannot be successfully treated by non-surgical means, such as the use of braces or physical therapy, revision surgery may be required.
Leg Fractures
The type and extent of the fracture will determine whether revision surgery is necessary. Revision surgery may be required if periprosthetic fractures (fractures around knee implants) compromise implant fixation or stability.
Stiffness
In some cases, a total knee replacement may not allow you to achieve the range of motion necessary to perform your daily activities. This can happen if excess scar tissue builds up around the knee, preventing the joint from fully moving. When this occurs, some patients may benefit from manipulating the knee under anesthesia. For this procedure, the patient returns to the operating room and the surgeon uses his or her hands to physically flex and straighten the knee to help it regain flexibility. If excess scar tissue has accumulated around the knee joint and has significantly impaired movement and has not been very successful with manipulation, revision surgery may be considered to allow you to regain movement to perform your daily activities.
How is a Failed Knee Replacement Treated?
When a knee replacement fails, I will provide non-surgical conservative treatment options whenever possible. The following treatments can be used to help relieve your symptoms:
- Rest
- Activity modification
- Physical therapy
- Supporting the knee for additional support
- Using non-steroidal anti-inflammatory drugs (NSAIDs)
Therefore, nonsurgical treatment is the treatment of choice when there is no clear diagnosis of residual pain. When pain is of moderate to severe quality and there is a clear diagnosis of implant failure, revision joint replacement surgery can help relieve pain and restore knee function. One or more of the previously implanted prosthetic knee components are removed and replaced during revision surgery. Bone transplants, metal augments, and/or bone cement can be used to reinforce the residual bone, and new components will be connected around the joint.
Revision knee replacement surgery produces favorable long-term benefits for the majority of patients, providing pain and stiffness relief while enhancing stability and function. Revision surgery, on the other hand, maybe more prone to problems and may not last as long as a first knee replacement. If there is an infection, surgery is almost always required. The revision may need to be completed in two stages: one to remove the joint and allow time for the infection to heal, and one to replace the joint. This is called a "two-stage exchange arthroplasty." A single-stage infection exchange is possible, during which the infected implant is removed and the final revision is placed during the same surgery. We are currently investigating which approach is superior in terms of (1) eradicating the infection and (2) providing the greatest clinical benefit to patients.
Surgery Overview
The first step is the removal of the existing implant. If there has been significant bone loss, bone grafts may be required to fill these gaps. Bone grafts can be autografts (your bone tissue, taken from another part of your body) or an allograft (bone tissue from another person obtained from a bone bank). In some cases, metal wedges, wires, or screws can be used to strengthen the bone. Finally, specialized revision knee implants are inserted. Temporary drains can be placed to help prevent excessive swelling of the knee and are usually removed a few days after surgery. In addition, specialized negative pressure incisional dressings are also frequently used to improve wound healing, as they have been shown to decrease postoperative wound complications in high-risk patients. These dressings are usually attached to a small portable pump that stays on for about a week and keeps the wound protected and dry.
During
First, the old implant is removed and, if necessary, bone grafts are used to fill in the gaps where the bone has deteriorated. Then the new prosthesis is placed. The majority of revision total knee replacement surgeries take longer than original procedures (about two to three hours).
After
After a primary knee replacement, the postoperative treatment is quite similar. Physical therapy, blood management, pain medications as needed, antibiotics, and some form of blood clot prevention are all included. A brace or splint may be used to protect the joint after surgery.
Recovery
Physical rehabilitation can begin within 24 hours after the surgery and last up to three months in most situations. Some patients take longer to recover. In some cases, a protective weight-bearing or limiting the knee's range of motion is needed to promote proper healing. Therapy will generally continue for up to three months after surgery. Assistive devices, such as a walker or crutches, will be used early in the convalescent period, and patients will switch to using a cane or walking without any assistance as their condition improves.
Expectations After Surgery
Most patients who undergo revision procedures can expect good to excellent results. Although pain reduction and improved stability and function are predicted outcomes, full pain relief, and function restoration are not always feasible. Up to 20% of patients may still experience some pain after revision knee surgery. This can persist for several years after the procedure. In addition, recovery after revision total knee surgery is highly dependent on the condition and function of the knee before revision surgery.
Alternatives to Revision Surgery
Alternatives to revision knee surgery are rarely used, as they can sometimes be more complex and give worse results than revision surgery, but include fusion or amputation of the knee. The following alternatives are used depending on the severity of the problem affecting the knee:
- Arthrodesis (fusion) of the knee joint can relieve pain but at the expense of keeping the knee in a fixed position without flexion.
- Amputation can be used in extreme cases where the knee joint has a severe infection that cannot be eradicated.
Complications
Revision total knee replacement carries the same risks as any other surgical surgery. Because the procedure is longer and more complex than primary total knee replacement, it has a higher risk of complications. Before your surgery, your doctor will discuss each risk with you and take specific steps to help avoid potential complications. The following are some of the potential risks and consequences of revision surgery:
- Poor wound healing
- Reduced range of motion or stiffness in the knee.
- Infection in the wound or new prosthesis
- Bleeding
- Blood clots in the legs, which can travel to the lungs (pulmonary embolism)
- Bone fracture during surgery.
- Damage to nerves or blood vessels.
- Medical problems such as heart attack, lung complications, or stroke.