- Cardiology 84
- Dermatology 45
- Endocrinology 33
- ENT 16
- Fertility 190
- Gastroenterology 78
- General-Medicine 81
- Gynecology 80
- Hematology 19
- Infectious-Diseases 33
- Neurology 52
- Oncology 34
- Ophthalmology 23
- Orthopedics 69
- Pediatrics 31
- Procedure 23
- Public-Health 144
- Pulmonology 59
- Radiology 8
- Urology 68
- Wellness 161
- Woman-and-child 77
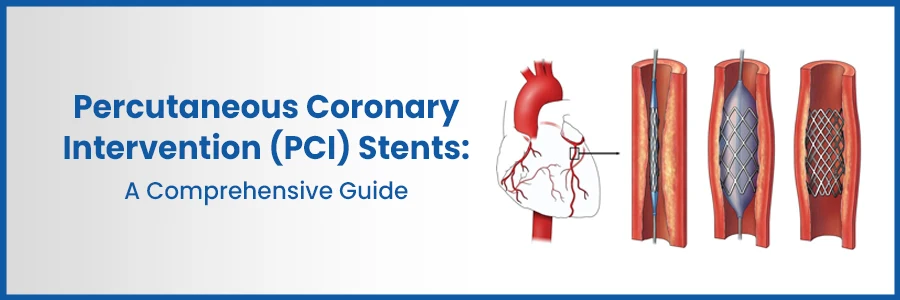
Percutaneous Coronary Intervention (PCI) Stents Guide
Percutaneous coronary intervention (PCI), also known as coronary angioplasty, is a minimally invasive procedure used to open narrowed or blocked coronary arteries, which are vital for supplying oxygen and nutrients to the heart muscle.
This procedure aims to alleviate symptoms like chest pain (angina) and shortness of breath and lower the risk of heart attack and stroke.
What is a PCI Stent?
A PCI stent is a small, expandable metal tube inserted into narrowed or blocked coronary arteries to maintain their openness. Stents, typically made of stainless steel, cobalt-chromium, or nickel-titanium, come in various sizes and lengths tailored to individual patient needs.
Get a second opinion from trusted experts and makeconfident, informed decisions.
Get Second OpinionTypes of PCI Stents
There are three primary types of PCI stents:
- Bare-metal stents: These stents are metal mesh tubes that expand to open the artery. They effectively widen narrowed arteries but carry a higher risk of restenosis, the re-narrowing of the artery.
- Drug-eluting stents: These stents release medication to reduce restenosis risk. They are recommended for higher-risk patients, such as those with diabetes or prior stent placements.
- Bioresorbable Vascular Scaffolds (BVS): BVS gradually dissolve over time, offering temporary support before being absorbed by the body.
Who Should Get PCI Stents?
PCI stents are recommended based on individual risk factors, including age, overall health, and severity of coronary artery disease. They are suitable for individuals with:
- Significant narrowing or blockage of one or more coronary arteries
- Symptoms like chest pain, shortness of breath, or fatigue
- History of heart attack or stroke
- Risk factors such as high blood pressure, high cholesterol, or diabetes
Who Should Not Have PCI Stents?
While PCI stents benefit many patients, they may not be suitable for those with:
- Active bleeding or severe bleeding disorders
- Severe allergies to contrast dye or stent materials
- Pregnancy or untreated high blood pressure
- Recent heart attack or stroke
Procedure Details
PCI stent procedures typically include these steps:
- Preparation: Patients are prepared by removing jewellery, receiving relaxation medication, and undergoing pre-procedure assessments.
- Catheter insertion: A thin, flexible tube (catheter) is inserted into the groin or wrist artery.
- Guidewire insertion: A guidewire is passed through the catheter to the narrowed artery.
- Balloon inflation: A balloon at the guidewire tip inflates to widen the artery.
- Stent placement: The stent is positioned over the narrowed area and expanded.
- Catheter removal: The balloon, guidewire, and catheter are withdrawn.
- Closure: The insertion site is closed with a small incision or bandage.
The entire procedure lasts about an hour, and patients are monitored post-procedure to prevent complications. Most can return home the same day.
Before Percutaneous Coronary Intervention Stent
Before the procedure, patients:
- Undergo thorough medical history reviews and diagnostic tests.
- May need to discontinue certain medications or fast.
During Percutaneous Coronary Intervention Stent
During the procedure:
- Local anesthesia is administered at the insertion site.
- Patients remain awake but sedated.
- A catheter with a deflated balloon and stent is guided to the blocked artery.
- The balloon inflates to compress plaque, and the stent is deployed to keep the artery open.
Your health is everything - prioritize your well-being today.
Schedule Your AppointmentBenefits of PCI Stents
PCI stents offer several benefits, including:
- Improved heart blood flow
- Reduced symptoms of coronary artery disease
- Lower risk of heart attack and stroke
- Minimally invasive procedure with shorter recovery time
Risks of PCI Stents
PCI stents carry potential risks, including:
- Bleeding, infection, or blood clot formation
- Artery damage or restenosis
Living with PCI Stents
Post-procedure, patients need to:
- Take medications to prevent stent-related blood clots
- Adopt lifestyle changes such as quitting smoking, a healthy diet, and regular exercise
- Attend regular follow-up appointments for monitoring
Frequently Asked Questions
Angioplasty is a broader time period referring to the dilation of blood vessels, at the same time as PCI (Percutaneous Coronary Intervention) especially entails catheter-primarily based approaches to treat narrowed or blocked coronary arteries.
No, Percutaneous Coronary Intervention (PCI) doesn't constantly involve a stent. While a stent is normally used to open blocked arteries, PCI can also consist of balloon angioplasty on my own without stent placement.
The three types of percutaneous coronary artery interventions are angioplasty, atherectomy, and stent placement. These procedures aim to open narrowed or blocked coronary arteries, restoring blood to the coronary heart.
The decision to locate a stent relies upon elements along with signs and symptoms, extent of blockage, and average fitness. Generally, stents are taken into consideration for massive blockages causing signs or high-threat conditions.
No, PCI is a minimally invasive system that uses a catheter and stent to open narrowed or blocked arteries, at the same time as bypass surgery involves growing new pathways for blood flow.
The manner usually takes about 30 to 60 mins, however the common time may additionally range based on character situations.
Most people can go home the same day of the procedure, and normal activities can often be resumed within a few days. However, individual recovery times may vary.
Yes, alternatives encompass medicinal drug management, lifestyle modifications, and in some cases, coronary artery bypass grafting (CABG). The choice depends on the individual's health condition and the severity of coronary artery sickness.

- Cardiology
- Case Studies
- Dermatology
- Endocrinology
- ENT
- Fertility
- Gastroenterology
- General
- General-Medicine
- Gynecology
- Hematology
- Infectious-Diseases
- Medical News
- Neurology
- Oncology
- Ophthalmology
- Orthopedics
- Pediatrics
- Procedure
- Public-Health
- Pulmonology
- Radiology
- Second Opinion
- Urology
- Wellness
- Woman-and-child