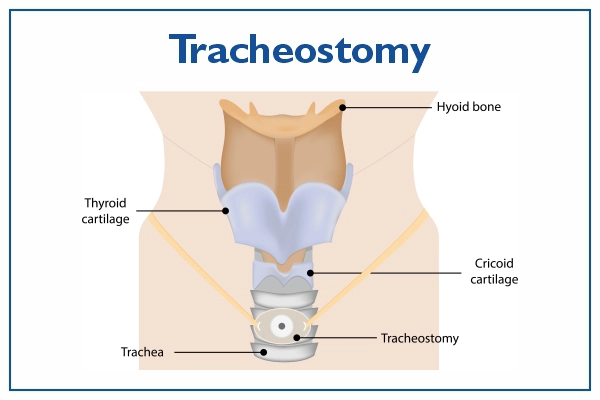
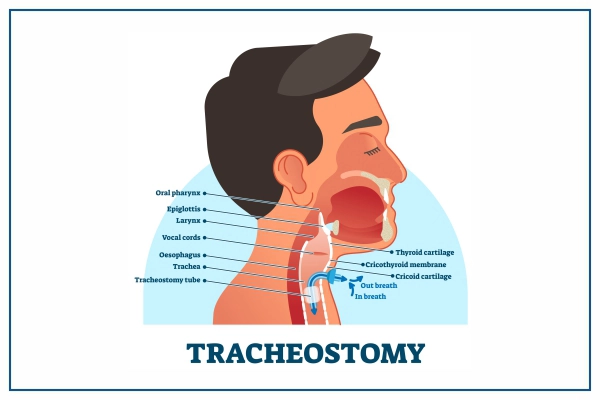
What is a Tracheostomy?
A tracheostomy, also known as tracheotomy, is a surgical procedure in which
a surgical opening, called a stoma, is created in the front of the neck and directly into the
trachea (windpipe). This opening provides an alternate and direct airway route for breathing,
bypassing the nose and mouth. A tracheostomy tube is inserted into this opening to maintain the
airway, allowing air to enter the lungs and facilitating ventilation. Tracheostomies are performed
for various medical reasons, including situations where a patient requires long-term or emergency
assistance with breathing, airway management, or removal of airway secretions.
Indications of the Tracheostomy
Tracheostomy procedures are performed for a variety of medical indications and
purposes, mainly centered around providing an alternate airway and facilitating breathing. Here are
some common indications and purposes of tracheostomy
- Airway Obstruction: Tracheostomies are often performed when there is a blockage or
obstruction in the upper airway due to conditions such as:
- Trauma or injury to the face or neck
- Tumors or growths in the throat or airway
- Severe inflammation or swelling of the airway, such as in cases of angioedema or
anaphylaxis
- Respiratory Distress: Tracheostomy can be indicated in situations of severe respiratory
distress, where the patient is unable to breathe effectively through the nose and mouth, and
immediate intervention is necessary to establish a secure airway.
- Long-Term Ventilation: Patients who require long-term mechanical ventilation,
often due to conditions like:
- Severe respiratory failure
- Neuromuscular disorders that affect respiratory muscles, such as ALS (Amyotrophic
Lateral Sclerosis) or muscular dystrophy
- Airway Protection: Tracheostomies can help protect the airway in cases of trauma or
burns to
the face, neck, or upper airway, when the normal route of breathing is compromised.
- Management of Secretions: Patients who are unable to clear their airways effectively
may
benefit from a tracheostomy, as it allows for easier suctioning and removal of secretions that
could
otherwise obstruct the airway.
- Weaning from Ventilation: In some cases, tracheostomy is performed to facilitate the
weaning
process from mechanical ventilation. It allows for gradual reduction of ventilator support as
the
patient's condition improves.
- Vocal Cord Paralysis: Tracheostomy may be considered in patients with bilateral
vocal cord
paralysis, as it provides a stable airway and can help prevent complications associated with
aspiration.
- Post-Operative Airway Support: After certain head and neck surgeries or surgeries
involving
the airway, a tracheostomy might be performed to ensure a safe and open airway during the
initial
healing phase.
- Coma or Unconsciousness: Patients in a coma or unconscious state who cannot maintain
their
own airway may require a tracheostomy to ensure adequate oxygenation and ventilation.
- Access for Procedures: A tracheostomy can serve as an access point for certain
medical
procedures, such as bronchoscopy or removal of airway foreign bodies.
Steps involved in a tracheostomy procedure:
Here are the general steps involved in a tracheostomy procedure:
- Preparation: The patient is positioned on the operating table, and anesthesia is
administered to ensure they are unconscious and pain-free during the procedure. In some cases,
local anesthesia and sedation might be used.
- Incision: A small horizontal or vertical incision is made in the skin of the lower
part of the neck, usually between the first and second or second and third tracheal rings.
- Exposure: The surgeon carefully separates the surrounding tissues, including the
muscles and blood vessels, to expose the trachea. Hemostasis (control of bleeding) is achieved
as needed.
- Tracheal Incision: A horizontal or vertical incision is made in the trachea itself,
between two tracheal rings. This incision allows direct access to the airway.
- Insertion of the Tracheostomy Tube: A tracheostomy tube, which is a specialized
medical device, is inserted into the tracheal incision. The tube has an outer cannula that
remains in the trachea and an inner cannula that can be removed and cleaned. The tube is
secured in place with ties or a collar.
- Verification of Placement: The surgeon ensures proper placement of the tracheostomy
tube by observing chest rise and fall, listening for breath sounds, and monitoring oxygen
saturation levels.
- Stabilization: The tracheostomy tube is secured in place using sutures or a
specialized tube holder. The skin incision is then closed with sutures or surgical staples.
- Dressing and Care: A sterile dressing is applied around the tracheostomy tube to
keep the area clean and prevent infection.
- Postoperative Care: Once the procedure is completed, the patient is taken to a
recovery area where they can wake up from anesthesia under medical supervision.
- Monitoring and Management: After the procedure, the patient's breathing, oxygen
levels, and vital signs are closely monitored. The tracheostomy tube is connected to a
ventilator if needed, and the patient's respiratory status is managed accordingly.
- Care and Maintenance: Regular cleaning of the tracheostomy site and tube, as well as
regular replacement of the inner cannula and any dressings, is crucial to prevent infection
and maintain airway function.
- Speech and Swallowing Therapy: In the days following the procedure, speech and
swallowing therapists may work with the patient to help them adapt to speaking and swallowing
with the tracheostomy tube in place.
- Decannulation: If the patient's condition improves and they no longer require the
tracheostomy tube, the tube can be removed in a process called decannulation.
Who will Treat for Tracheostomy Procedure
Several medical specialists are trained to perform tracheostomy procedures due
to their expertise in airway management, surgical skills, and understanding of the anatomy of the head
and neck. The specialists who commonly perform tracheostomies include
- Otolaryngologists (ENT Surgeons): Otolaryngologists, also known as ear, nose, and
throat ENT surgeons or otolaryngology-head and neck surgeons, have
specialized training in
disorders of the head and neck, including the upper airway. They are often the primary
specialists responsible for performing tracheostomy procedures. Their expertise in airway
anatomy and surgical techniques makes them well-suited for this procedure.
- Thoracic Surgeons: Thoracic surgeons specialize in surgical procedures involving
the chest, including the lungs and airways. They may be involved in performing tracheostomies,
especially in cases where the procedure is part of a larger surgical intervention or when the
patient's respiratory condition requires a higher level of expertise.
- Critical Care Physicians/Intensivists: Critical care physicians or intensivists are
specialists who manage critically ill patients in intensive care units (ICUs). They may
perform tracheostomies on patients who require prolonged mechanical ventilation and have
complex respiratory conditions. Intensivists have a deep understanding of airway management
and the medical needs of critically ill patients.
- Anesthesiologists: Anesthesiologists are experts in administering anesthesia and
managing patients' airways during surgical procedures. While they may not always be the
primary specialists performing tracheostomies, they can be involved, especially when the
procedure is done under general anesthesia in an operating room.
- Oral and Maxillofacial Surgeons: These surgeons specialize in treating conditions
related to the mouth, jaws, and face. In certain cases, they may be involved in performing
tracheostomies, particularly if the procedure is combined with facial trauma reconstruction or
other oral and maxillofacial procedures.
- Trauma Surgeons: In emergency situations, trauma surgeons may perform
tracheostomies as part of life-saving interventions for patients with compromised airways due
to traumatic injuries.
Preparing for Tracheostomy procedure
Preparing for a tracheostomy procedure involves thorough assessment, planning,
and coordination among healthcare professionals. Here's a general outline of how to prepare for a
tracheostomy procedure:
- Medical Evaluation:
- The patient's medical history, current condition, and respiratory status are assessed
to determine the need for a tracheostomy.
- Diagnostic tests such as X-rays, CT scans, and blood tests may be
performed to gather
essential information.
- Informed Consent:
- The patient or their legal guardian is informed about the procedure, its risks,
benefits, and potential complications.
- The patient's questions and concerns are addressed, and informed consent is obtained.
- Preoperative Assessment:
- A thorough physical examination is conducted to evaluate the patient's overall health
and airway anatomy.
- Existing medical conditions, allergies, medications, and anesthesia considerations are
reviewed.
- Nutrition and Hydration: Adequate nutrition and hydration are ensured before the
procedure to support the patient's overall well-being and recovery.
- Medication Management: Medications that may affect bleeding or clotting are
reviewed, and adjustments may be made in consultation with the healthcare team.
- Discussion with Specialists: Depending on the patient's medical condition,
specialists such as anesthesiologists, critical care physicians, or surgeons may be consulted
to optimize the care plan.
- Communication and Coordination: The healthcare team, including surgeons, nurses,
anesthesiologists, and respiratory therapists, collaborates to
develop a comprehensive plan
for the procedure and post-operative care.
- Preoperative Instructions:
- Patients are given specific instructions about fasting before the procedure, which
helps prevent complications during anesthesia.
- Any necessary medications are taken as instructed by the healthcare team.
- Preparation for Anesthesia: If the procedure requires general anesthesia, patients
are prepared for anesthesia induction and intubation before the tracheostomy is performed.
- Consent Forms and Documentation: Consent forms are signed, and necessary
documentation is completed to ensure legal and ethical compliance.
- Patient and Family Education: Patients and their families are educated about what
to expect before, during, and after the procedure, including potential complications, care of
the tracheostomy tube, and recovery.
- Psychosocial Support: Patients and families may receive emotional support and
counseling to address concerns and alleviate anxiety.
- Preoperative Hygiene: The surgical site and surrounding areas are cleaned as part
of infection prevention measures.
- Equipment and Supplies: The necessary tracheostomy kit, sterile drapes, and other
medical supplies are prepared for the procedure.
Recovery after Tracheostomy procedure
Recovery after a tracheostomy procedure involves a combination of medical care,
monitoring, and patient education. The goal is to ensure proper healing of the surgical site, prevent
complications, and facilitate the patient's transition to using the tracheostomy tube for breathing.
Here's what to expect during the recovery period:
- Immediate Postoperative Period:
- The patient is closely monitored as they wake up from anesthesia.
- Vital signs, including heart rate, blood pressure, and oxygen levels, are regularly
checked.
- Ventilation and oxygenation are assessed to ensure proper functioning of the
tracheostomy tube.
- Pain management is provided if necessary.
- Tracheostomy Tube Care:
- The healthcare team will provide instructions on how to care for the tracheostomy tube,
including cleaning and suctioning techniques.
- Proper hygiene around the stoma site is emphasized to prevent infection.
- Suctioning is performed as needed to clear secretions and maintain airway patency.
- Communication and Mobility:
- Patients are educated on how to communicate while using a tracheostomy tube. Writing,
gesturing, or using communication devices may be helpful.
- Patients are encouraged to move and ambulate, as long as it's safe and doesn't disrupt
the tracheostomy tube.
- Swallowing and Eating:
- Patients may need to temporarily modify their diet and swallowing techniques to prevent
aspiration and ensure safe eating.
- If the patient's condition allows, they may start oral intake under the guidance of a
speech therapist.
- Breathing and Weaning:
- Depending on the patient's respiratory condition, weaning from mechanical ventilation
may begin gradually once they're stable.
- The healthcare team will closely monitor the patient's ability to breathe on their own
and adjust ventilator settings as needed.
- Tracheostomy Tube Changes:
- The initial tracheostomy tube may need to be changed after a certain period, typically
within the first week, to prevent tube obstruction and ensure proper fit.
- Subsequent tube changes will be based on the patient's progress and condition.
- Speech and Rehabilitation:
- Speech therapists may be involved to help patients regain or develop communication
skills while using a tracheostomy tube.
- Rehabilitation programs may be recommended to improve overall respiratory function and
muscle strength.
- Follow-Up Appointments: Patients will have regular follow-up appointments with the
healthcare team to monitor their progress, adjust care plans, and assess the need for further
interventions.
- Transition to Home Care:
- If the patient is stable and their condition allows, they may transition to home care
with the tracheostomy tube. Caregivers are educated on proper tube care and emergency
procedures.
- Home healthcare services may be arranged if necessary.
Lifestyle changes after Tracheostomy procedure
Undergoing a tracheostomy procedure will lead to certain lifestyle changes to
ensure proper care of the tracheostomy tube and to adapt to the new way of breathing. These changes
are essential to prevent complications and maintain optimal respiratory function. Here are some common
lifestyle changes that individuals may need to make after a tracheostomy procedure:
- Tracheostomy Tube Care:
- Learn and follow proper tracheostomy tube care techniques, including cleaning,
suctioning, and maintaining hygiene around the stoma site.
- Understand the signs of infection and monitor the stoma site for redness, swelling,
discharge, or unusual odors.
- Breathing and Ventilation:
- Adjust to breathing through the tracheostomy tube. Breathing may feel different
initially, but many patients adapt over time.
- Follow ventilator settings and recommendations from healthcare professionals if
mechanical ventilation is required.
- Mobility and Activities:
- Continue to move and engage in activities as allowed by the healthcare team. Being
active can help maintain overall health and lung function.
- Be cautious with physical activities that could disrupt the tracheostomy tube or cause
injury.
- Communication:
- Adapt to new communication methods, such as using gestures, writing, or communication
devices.
- Consider using speaking valves or devices that allow air to pass over the vocal cords
for improved speech.
- Swallowing and Eating:
- Follow recommendations from speech therapists or healthcare professionals for safe
swallowing and eating.
- Modify the diet if necessary to prevent aspiration and choking risks.
- Hydration and Nutrition:
- Ensure adequate hydration and nutrition to support healing and overall well-being.
- Work with healthcare professionals to determine the appropriate diet based on
individual needs.
- Social and Emotional Well-being:
- Address any emotional or psychological adjustments related to the tracheostomy with
support from family, friends, and mental health professionals.
- Engage in activities that bring joy and maintain social connections.
- Emergency Preparedness:
- Learn how to handle emergency situations involving the tracheostomy tube, such as
dislodgement or blockage, and have a plan in place.
- Ensure caregivers, family members, or close contacts are also educated about emergency
procedures.
- Follow-Up Appointments: Attend all scheduled follow-up appointments with the
healthcare team to monitor progress, make any necessary adjustments, and address concerns.
- Follow-Up Appointments: Attend all scheduled follow-up appointments with the
healthcare team to monitor progress, make any necessary adjustments, and address concerns.
- Travel and Accessibility:
- Plan ahead for travel, ensuring that necessary supplies, equipment, and medical
information are readily available.
- Communicate with airlines, hotels, and other accommodations about any special needs
related to the tracheostomy.
- Self-Care and Independence: Learn to care for the tracheostomy tube independently,
as much as possible, to promote self-sufficiency.