What is Tooth Extraction?
Tooth extraction or Dental Extraction is a process of extracting or removing the tooth from its socket in the jawbone. Numerous conditions, such as severe tooth decay, gum disease, crowding, trauma, infections, or orthodontic treatment preparation may call for this operation.
Indications of Tooth Extraction Procedure
Tooth extraction is recommended in various situations when a tooth cannot be saved or poses a risk to your oral health. The decision to perform a tooth extraction is typically made after careful evaluation by a dentist or oral surgeon. Here are the common indications for a tooth extraction procedure:
-
Severe Tooth Decay: When tooth decay has progressed to an extent that the tooth's structure is severely compromised, extraction may be necessary.
-
Advanced Gum Disease (Periodontal Disease): Gum disease can cause the supporting structures around the tooth to weaken, which may result in tooth extraction if it becomes loose.
-
Impacted Wisdom Teeth: Wisdom teeth, or third molars, often lack sufficient space to emerge properly. Impacted wisdom teeth can cause pain, infection, damage to adjacent teeth, and other complications.
-
Overcrowding: Orthodontic treatment, such as braces, may require the extraction of a tooth to create space for proper alignment of teeth.
-
Trauma or Fractures: Teeth that have sustained severe trauma or fractures that cannot be effectively repaired may need to be extracted.
-
Infection or Abscess: To stop the infection from spreading, a tooth infection that cannot be treated with root canal therapy may need to be pulled.
-
Risk of Infection: In some cases, teeth with a high risk of infection, especially in individuals with compromised immune systems, may be extracted as a preventive measure.
-
Preparing for Orthodontic Treatment: Teeth that hinder proper orthodontic treatment, such as severely misaligned teeth, may be extracted to facilitate orthodontic procedures.
-
Malpositioned Teeth: Teeth that are misaligned, rotated, or positioned in a way that affects your bite or oral function might require extraction.
-
Non-Restorable Teeth: If a tooth is extensively damaged due to decay, trauma, or other factors and cannot be restored with dental treatments, extraction may be the best option.
-
Supernumerary Teeth: Extra teeth that cause crowding, impact other teeth, or hinder proper oral function may be extracted.
-
Prior to Radiation or Organ Transplant: If you're undergoing radiation therapy to the head or neck, or if you're preparing for an organ transplant, teeth in the treatment area may need to be extracted to reduce the risk of infection.
-
Baby Teeth That Don't Fall Out: Sometimes, baby teeth don't naturally fall out, obstructing the eruption of permanent teeth. Extraction might be necessary to allow the permanent teeth to emerge.
Secure your health with a second opinion. Make informed decisions and book your appointment today!
Get A Second Opinion
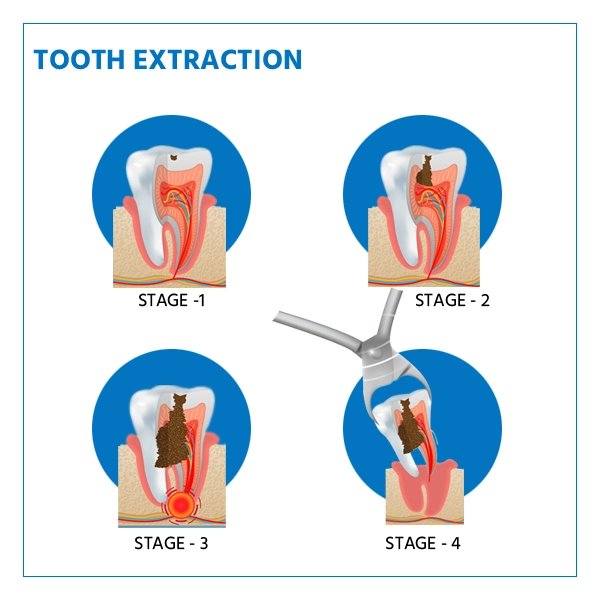
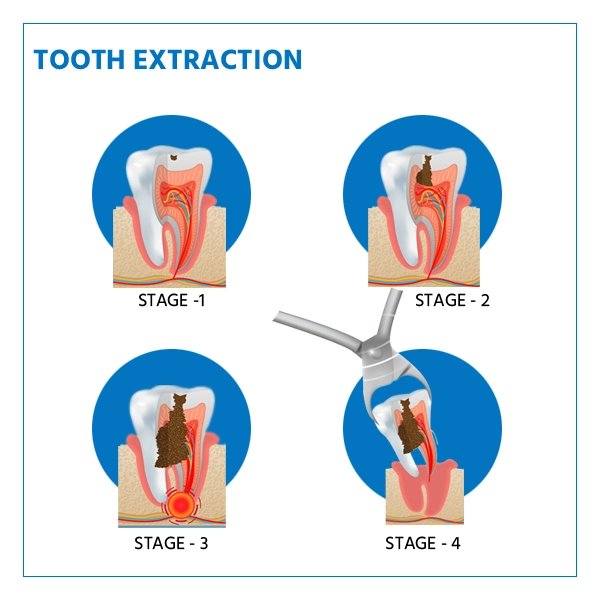
Steps involved in Tooth Extraction Procedure
The tooth extraction procedure involves several steps to safely and effectively remove a tooth from its socket in the jawbone.
Here's a detailed overview of what typically happens during a tooth extraction:
-
Diagnosis and Assessment: The dentist conducts a thorough examination of your oral health, including X-rays or other imaging to assess the tooth's condition, root structure, and surrounding bone. This helps determine the best approach for the extraction.
-
Preoperative Preparation: The dentist discusses the procedure with you, explaining the reasons for extraction, potential complications, and available options. Your medical history, including any medications you're taking, is reviewed to ensure your safety during the procedure.
-
Anesthesia: Local anesthesia is administered to numb the area around the tooth to ensure you won't feel pain during the extraction. In some cases, additional sedation options like nitrous oxide (laughing gas) or oral sedatives might be used to help you relax.
-
Tooth Extraction: The actual extraction process begins with the dentist or oral surgeon using specialized instruments to gently and carefully loosen the tooth from its socket. Depending on the tooth's condition and location, the dentist might need to use forceps or elevators to wiggle the tooth back and forth, gradually loosening it.
-
Sectioning (if necessary): In some cases, a tooth might be too large or have complex root shapes. The dentist might need to carefully section the tooth into smaller pieces for easier removal.
-
Socket Cleaning: After the tooth is extracted, the socket (the space left behind in the jawbone) may be cleaned to remove any infected tissue, debris, or bone fragments.
-
Gauze and Blood Clot Formation: To promote healing and prevent excessive bleeding, the dentist places a piece of sterile gauze over the extraction site and asks you to bite down. This pressure helps a blood clot form in the socket.
-
Suturing (if necessary): Depending on the case, the dentist might place sutures to close the wound and aid in proper healing. Sutures are often used for complex extractions or to control bleeding.
-
Post-Extraction Instructions: The dentist provides you with detailed post-operative instructions, including how to care for the extraction site, what foods to avoid, and how to manage discomfort. Pain medications and antibiotics may be prescribed if needed.
-
Recovery and Healing: Over the next few days, a blood clot forms in the socket. This clot is crucial for healing and preventing complications like dry socket.
-
Follow-up Appointment: A follow-up appointment may be scheduled to monitor your healing progress and remove sutures if they were placed.
-
Replacement Options (if applicable): Depending on the tooth's location and your dental needs, the dentist might discuss replacement options like dental implants, bridges, or dentures.
Who will Treat for Tooth Extraction Procedure
Tooth extraction procedures are typically performed by Dentists or Oral Surgeons. The choice of who will treat you depends on the complexity of the extraction, your specific oral health needs, and the preferences of your dental care provider.
Here's a breakdown of the professionals who might be involved in your tooth extraction procedure:
-
Dentists
-
General Dentists: Many routine tooth extractions, especially those involving non-complicated teeth, are performed by general dentists. They are skilled in various dental procedures and have experience in simple extractions.
-
Family Dentists: Similar to general dentists, family dentists can perform routine tooth extractions.
-
Pediatric Dentists (Pedodontists): Pediatric dentists specialize in treating children's dental needs, including tooth extractions for kids.
-
Prosthodontists: Prosthodontists focus on restoring and replacing missing teeth. They may be involved in more complex extraction cases, especially when it's part of a larger treatment plan.
-
Oral Surgeons: Oral surgeons are dental specialists who have completed additional years of education and training beyond dental school. They specialize in surgical procedures related to the mouth, jaw, and face. Oral surgeons are typically involved in more complex extractions, including impacted wisdom teeth, surgical extractions, and cases requiring anesthesia.
-
Anesthesiologists: For more complex extractions or cases involving general anesthesia or deep sedation, an anesthesiologist or nurse anesthetist might be involved to ensure your comfort and safety during the procedure.
Preparing for Tooth Extraction Procedure
There are a number of actions you can do to get ready for a tooth extraction to make sure everything goes smoothly and you're comfortable.
Here's a guide on how to prepare for a tooth extraction:
-
Consultation with Your Dentist: Schedule a consultation with your dentist to discuss the need for the extraction and your oral health history. They will evaluate the tooth's condition, take X-rays if necessary, and determine the best approach for the procedure.
-
Share Your Medical History: Inform your dentist about any medical conditions you have, medications you're taking (including over-the-counter drugs and supplements), and allergies. This information helps ensure your safety during the procedure.
-
Discuss Anesthesia Options: If you're anxious about the procedure, discuss anesthesia options with your dentist. They can explain local anesthesia, nitrous oxide (laughing gas), or oral sedation to help you relax during the extraction.
-
Arrange Transportation: If you'll receive any form of sedation or anesthesia that impairs your ability to drive, arrange for someone to drive you to and from the appointment.
-
Follow Preoperative Instructions: Your dentist will provide specific instructions to follow before the procedure. This might include fasting if sedation will be used, as well as guidelines for taking any prescribed medications.
-
Food and Drink: If you're receiving sedation, follow your dentist's instructions about when to stop eating and drinking before the procedure. Typically, you'll need to avoid food and drink for several hours before the appointment.
-
Dress Comfortably: Wear comfortable clothing to the appointment. Loose-fitting clothing with short sleeves is ideal, as it allows for easy access to your arm for the administration of intravenous medications if needed.
-
Arrange Post-Procedure Care: Plan for someone to assist you after the procedure, especially if you receive sedation or anesthesia. You might not be in a condition to drive or perform certain tasks immediately after the extraction.
-
Post-Extraction Supplies: Your dentist might recommend purchasing over-the-counter pain relievers, gauze, and any prescribed medications ahead of time so you have them available after the procedure.
-
Ask Questions: In case you have any questions about the procedure, anesthesia, aftercare, or recovery, don't hesitate to ask your dentist during the consultation.
-
Hygiene: On the day of the procedure, brush and floss your teeth as usual. The Infection risk can be reduced by practising Good oral hygiene helps.
-
Relaxation Techniques: If you're feeling nervous, some practice relaxation techniques such as deep breathing or mindfulness to help calm your nerves.
-
Bring Identification and Insurance Information: Have your identification and insurance information ready for the appointment, if applicable.
Ready to take control of your health journey? Book your appointment now and start your path towards wellness today!
Book an Appointment
Recovery after Tooth Extraction Procedure
Recovery after a tooth extraction procedure is an important phase that requires proper care to ensure optimal healing and minimize complications.
Here's a general guide to what you can expect during the recovery process:
-
Immediate Post-Extraction Period:
-
Bite on a Gauze Pad: Your dentist will place a piece of sterile gauze over the extraction site and ask you to bite down firmly. This helps form a blood clot, which is essential for proper healing.
-
Rest: Take it easy for the rest of the day after the procedure. Avoid strenuous activities that could dislodge the blood clot.
-
Avoid Rinsing or Spitting: Avoid rinsing your mouth or spitting vigorously on the day of the extraction. This can disturb the blood clot and delay healing.
-
Pain and Discomfort: Some discomfort, swelling, and mild pain around the extraction site are normal. Over-the-counter pain relievers prescribed by your dentist can help manage pain.
-
Swelling: Swelling around the extraction site may occur. Applying an ice pack to the area for 20-minute intervals can help reduce swelling during the first 24 hours.
-
Diet: Stick to a soft or liquid diet for the first day or two after the procedure. Avoid foods which are hot, spicy, or crunchy as they may irritate the extraction site.
-
Oral Hygiene: Continue brushing your teeth gently, but avoid the extraction area. Be cautious around the site to prevent dislodging the blood clot.
-
Avoid Smoking and Alcohol: Refrain from smoking and drinking alcohol for at least the first 24 hours after the extraction. Both activities can hinder the healing process.
-
Pain Medications: Take any prescribed pain medications as directed by your dentist to manage discomfort.
-
Follow-Up Appointments: Attend any scheduled follow-up appointments to ensure proper healing and address any concerns.
-
Healing Time: The initial healing period typically lasts a few days. Complete healing of the extraction site may take a few weeks, depending on the complexity of the extraction.
-
Dry Socket Prevention: Avoid activities that could lead to dry socket, a painful condition that occurs when the blood clot dislodges prematurely. This includes not using straws, smoking, or engaging in vigorous rinsing.
-
Resuming Normal Activities: After the first day, gradually return to your normal activities while being cautious around the extraction site.
-
Signs of Complications: Contact your dentist if you experience severe pain, excessive bleeding, signs of infection (fever, swelling, foul taste), or if you have concerns about the healing process.
-
Follow Post-Extraction Care Instructions: Follow all the post-extraction care instructions provided by your dentist. Proper care can help prevent complications and promote smooth healing.
Lifestyle changes after Tooth Extraction Procedure
After a tooth extraction procedure, making certain lifestyle adjustments can help promote optimal healing, prevent complications, and ensure your overall well-being.
Here are some lifestyle changes to consider after undergoing a tooth extraction:
-
Diet Modifications: Stick to a soft or liquid diet for the first few days after the extraction. Avoid hot, spicy, crunchy, and hard foods that could irritate the extraction site. Gradually reintroduce solid foods as you feel comfortable.
-
Hydration: Stay well-hydrated by drinking water and fluids that are not too cold or too hot. Hydration supports overall healing and helps prevent dry mouth.
-
Avoid Straws and Sucking: Refrain from using straws or engaging in activities that involve sucking through a straw. These actions can dislodge the blood clot and lead to a dry socket.
-
Smoking and Tobacco Cessation: If you're a smoker, consider quitting or at least avoid smoking for several days after the extraction. Smoking can hinder the healing process and increase the risk of complications.
-
Alcohol Avoidance: Avoid alcohol consumption for at least the first 24 hours after the procedure, as it can interfere with blood clot formation and healing.
-
Oral Hygiene: Continue practicing good oral hygiene, but be gentle around the extraction site. Avoid brushing directly on the site for the first few days. Rinse your mouth gently with warm saltwater after the first 24 hours.
-
Physical Activity: While you should avoid strenuous activities immediately after the extraction, light to moderate physical activity can promote blood circulation and healing. Consult your dentist for specific guidance.
-
Rest and Recovery: Allow your body ample time to rest and recover after the procedure. Avoid overexertion and get enough sleep to support healing.
-
Medication Adherence: If your dentist prescribed pain medications, antibiotics, or other medications, take them as directed to manage discomfort and prevent infection.
-
Follow-Up Appointments: Attend any scheduled follow-up appointments to ensure proper healing and address any concerns.
-
Nutritional Support: Consume a balanced diet rich in vitamins and nutrients to support the healing process. Include foods that are soft and easy to chew.
-
Avoid Biting or Chewing Near the Extraction Site: Avoid chewing directly on the extraction site until it has fully healed to prevent irritation or disruption of the healing process.
-
Monitor Healing: Keep an eye on the extraction site for signs of infection, excessive bleeding, or delayed healing. If you notice anything unusual, contact your dentist.
-
Stress Reduction: Manage stress through relaxation techniques such as deep breathing, meditation, or gentle exercise. Stress can affect your body's ability to heal.
-
Follow Your Dentist's Recommendations: Your dentist will provide specific post-extraction care instructions. Follow these guidelines closely to ensure a smooth recovery.