What is Surgical Aortic Valve Replacement (SAVR)?
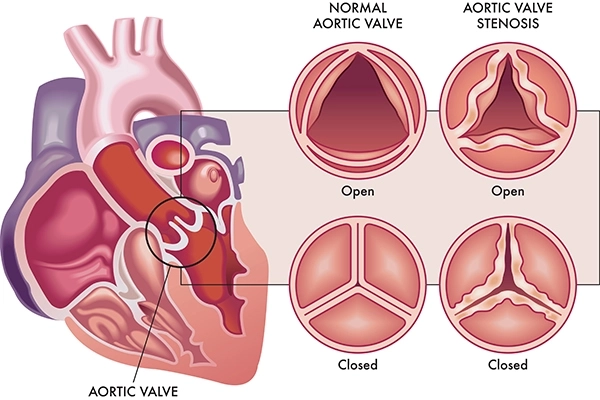
Surgical Aortic Valve Replacement (SAVR) is a well-established and effective medical procedure designed to treat aortic valve disease, affecting the heart's ability to pump blood efficiently. The aortic valve, a crucial component of the heart, regulates the flow of oxygen-rich blood from the heart to the rest of the body. When this valve becomes diseased or narrowed (aortic stenosis), it can lead to chest pain, shortness of breath, and fatigue.
Indications of Surgical Aortic Valve Replacement (SAVR) Procedure:
Surgical Aortic Valve Replacement (SAVR) is a procedure primarily indicated for individuals with severe aortic valve disease, specifically aortic stenosis or aortic regurgitation, where the aortic valve becomes narrowed or leaky. The decision to undergo SAVR is based on a thorough cardiac surgeon and medical team evaluation. Indications for SAVR include:
- Severe Aortic Stenosis : When the aortic valve becomes significantly narrowed, restricting blood flow from the heart into the aorta and the rest of the body, it can lead to symptoms like chest pain, shortness of breath, fatigue, and fainting. SAVR is often recommended to alleviate these symptoms and improve overall heart function.
- Severe Aortic Regurgitation : Aortic regurgitation occurs when the aortic valve does not close properly, allowing blood to leak back into the heart. This can lead to an enlarged heart and reduced pumping efficiency. SAVR may be considered to repair or replace the valve and restore proper blood flow.
- Symptomatic Patients : SAVR is often recommended for patients who experience significant symptoms, such as severe fatigue, breathlessness, chest pain, or fainting, due to aortic valve disease.
- Reduced Heart Function : If aortic valve disease has significantly decreased heart function, SAVR may be recommended to improve cardiac output and overall cardiovascular health.
- Disease Progression : When aortic valve disease progresses rapidly or becomes increasingly severe, surgical intervention may be necessary to prevent further deterioration and complications.
- Failed Previous Interventions : Patients who have previously undergone other procedures, such as aortic valve repair or less invasive interventions like Transcatheter Aortic Valve Replacement (TAVR), and have experienced treatment failure or valve dysfunction may be candidates for SAVR.
- Combined Procedures : SAVR may be considered in combination with other heart procedures, such as coronary artery bypass grafting (CABG), for patients with multiple cardiac issues.
Steps involved in Surgical Aortic Valve Replacement (SAVR) Procedure:
Surgical Aortic Valve Replacement (SAVR) is a complex procedure performed by a team of skilled cardiac surgeons, anesthesiologists, and other medical professionals. It involves several key steps to replace a diseased or malfunctioning aortic valve with a prosthetic valve. Here's an overview of what happens during a SAVR procedure:
- Anesthesia : The patient is put under general anaesthesia to ensure they are unconscious and pain-free during the surgery.
- Incision : A surgical incision is made in the chest, typically through the sternum (breastbone). This grants access to the heart and aorta.
- Cardiopulmonary Bypass (Heart-Lung Bypass) : The patient's blood circulation is rerouted from the heart and lungs to a heart-lung machine. This machine takes over the function of pumping blood and oxygenating it, allowing the surgeon to work on the heart while it's not actively pumping.
- Cooling the Body : In some cases, the patient's body temperature is lowered to reduce the body's oxygen demand and protect the organs during the temporary suspension of blood circulation.
- Opening the Heart : The surgeon carefully opens the heart's chambers to access the aortic valve.
- Removal of the Diseased Valve : The damaged or diseased aortic valve is removed from its position.
- Sizing and Placement : The surgeon measures the size of the patient's annulus (the base of the aorta where the valve sits) to determine the appropriate size of the prosthetic valve.
- Suturing the New Valve : The prosthetic valve (typically made of bioprosthetic or mechanical materials) is securely sewn into the annulus, replacing the original valve's function.
- Closing the Heart : Once the new valve is in place and functioning correctly, the heart's chambers are closed, and the seat can resume pumping.
- Separation from the Heart-Lung Bypass Machine : The patient's blood circulation is gradually returned to the heart, and the heart-lung machine is disconnected.
- Closing the Incision : The surgical incision is closed with sutures or staples. The sternum may be wired together to promote proper healing.
- Recovery and Monitoring : The patient is transferred to the intensive care unit (ICU) for close monitoring during the initial stages of recovery. Vital signs, heart function, and other parameters are closely observed.
- Postoperative Care : Once stable, the patient is moved to a regular hospital room for further recovery. Pain management, wound care, and rehabilitation begin.
- Rehabilitation and Discharge : Physical therapy and rehabilitation help the patient regain strength and mobility. The length of the hospital stay varies, but it typically lasts around a week.
- Follow-up : After discharge, the patient will have regular follow-up appointments with their medical team to monitor their progress, assess the functioning of the new valve, and ensure proper recovery.
Who will Treat for Surgical Aortic Valve Replacement (SAVR) Procedure:
Surgical Aortic Valve Replacement (SAVR)" is a complex cardiac surgical procedure typically performed by a specialized team of medical professionals, primarily a cardiac surgeon. Here are the key individuals who may be involved in the treatment process:
- Cardiac Surgeon : A cardiac surgeon is a specialized surgeon trained in performing surgical procedures on the heart and its blood vessels. They are the primary healthcare professionals responsible for carrying out the SAVR procedure. Cardiac surgeons have extensive expertise in cardiac anatomy, surgical techniques, and patient management.
- Cardiologist : Cardiologists are specialized physicians who diagnose and treat heart conditions. They are crucial in assessing the patient's overall cardiac health, determining the need for SAVR, and coordinating with the cardiac surgeon to provide comprehensive care.
- Anesthesiologists : Anesthesiologists are responsible for administering anaesthesia to the patient before the surgery, monitoring their vital signs, and ensuring their comfort and safety throughout the surgical process.
- Perfusionist : Perfusionists operate the heart-lung bypass machine during the SAVR procedure. They manage the machine that takes over the functions of the heart and lungs, maintaining oxygenation and circulation of the patient's blood while the heart is temporarily stopped.
- Nurse Practitioners and Physician Assistants : These healthcare professionals assist in patient care before, during, and after the surgery. They may provide education, manage postoperative care, and communicate with the patient and their family members.
- Surgical Team : This includes surgical nurses, scrub nurses, and other surgical team members who assist the cardiac surgeon during the procedure by handing instruments, managing equipment, and ensuring a sterile surgical environment.
- Cardiovascular Imaging Specialists : These specialists may be involved in assessing the patient's cardiac imaging, such as echocardiograms and angiograms, to provide detailed information about the condition of the aortic valve and surrounding structures.
- Rehabilitation Team : After the surgery, a team of physical therapists, occupational therapists, and other rehabilitation specialists work together to help the patient recover strength, mobility, and overall function.
- Social Workers and Counselors : These professionals offer emotional support, counselling, and assistance in managing the psychological and emotional aspects of undergoing major cardiac surgery.
- Nutritionists and Dietitians : They guide postoperative dietary needs and nutritional considerations to support the patient's recovery and overall heart health.
- Pulmonologist : In cases where lung function may be compromised, a pulmonologist may be consulted to assess lung health and provide recommendations to optimize respiratory function before and after surgery.
- Medical Support Staff : This includes administrative staff, medical technologists, and other support personnel who ensure the smooth operation of the surgical unit and provide assistance as needed.
Preparing for Surgical Aortic Valve Replacement (SAVR) Procedure:
Preparing for Surgical Aortic Valve Replacement (SAVR) involves thorough planning, medical evaluations, and lifestyle adjustments to ensure a safe and successful procedure and recovery. Here's how to prepare:
- Consultation with Cardiologist and Surgeon : Schedule consultations with your cardiologist and cardiac surgeon. They will assess your overall health, discuss the need for SAVR, and provide you with information about the procedure, potential risks, and benefits.
- Medical Evaluation : Undergo a comprehensive medical evaluation, including blood tests, imaging studies (echocardiogram, angiogram, etc.), and other assessments to determine your overall health status and suitability for surgery.
- Discuss Medications : Inform your medical team about all the medications you are currently taking, including prescription drugs, over-the-counter medications, supplements, and herbal remedies. They will advise you on medications to continue or adjust before the surgery.
- Smoking and Alcohol : If you smoke or consume alcohol, consider quitting or reducing these habits before the surgery. Smoking and excessive alcohol consumption can affect healing and increase surgical risks.
- Nutrition and Hydration : Eat a balanced diet of nutrients to support your immune system and overall health. Stay hydrated and maintain a healthy weight.
- Physical Activity : Engage in light to moderate physical activity if your health permits. Staying physically active can help improve your fitness and prepare your body for surgery.
- Dental Care : Address any dental issues, infections, or treatments before the surgery to reduce the risk of disease.
- Vaccinations : Ensure your vaccinations are up-to-date. Your medical team may recommend specific vaccinations to reduce the risk of infections.
- Medication Adjustments : Your medical team may adjust your medications before the surgery, especially if you take anticoagulants or blood-thinning drugs.
- Blood Donation : Some patients may be advised to donate their blood in case a blood transfusion is needed during or after the surgery.
- Preoperative Testing : Complete any required preoperative tests or consultations, such as a meeting with an anesthesiologist.
- Education and Questions : Attend sessions about the SAVR procedure, its risks, benefits, and expected outcomes. Ask any questions you have to clarify your understanding.
- Legal and Financial Matters : Review and complete any necessary legal and financial documentation related to the surgery, such as consent forms and insurance arrangements.
- Advance Directives : Consider creating advance directives or living wills to communicate your preferences for medical care in case you cannot make decisions during recovery.
- Support System : Arrange for a support system, such as a family member or friend, who can assist you before and after the surgery.
- Home Preparation : Prepare your home environment for your recovery. Create a comfortable space with necessary supplies, including a recliner or comfy chair, loose clothing, and toiletries.
- Transportation : Arrange transportation to and from the hospital for the day of the surgery and follow-up appointments.
- Fasting and Medication Guidelines : Follow specific fasting and medication guidelines provided by your medical team before the surgery.
- Emotional Preparation : Practice relaxation techniques, meditation, or mindfulness to manage pre-surgery anxiety and stress.
- Follow Instructions : Adhere to all preoperative instructions from your medical team to ensure a smooth and safe surgical experience.
Recovery after Surgical Aortic Valve Replacement (SAVR) Procedure:
Recovery after Surgical Aortic Valve Replacement (SAVR) is a gradual process involving healing, regaining strength, and returning to normal activities. The timeline and experience can vary for each individual, but here's a general overview of what to expect during the recovery period:
Immediate Postoperative Period (In Hospital):
- Intensive Care Unit (ICU) : After the surgery, you will be closely monitored in the ICU for the first few days. Medical staff will closely monitor your heart function, vital signs, and overall condition.
- Ventilation : Initially, you may be connected to a ventilator to help with breathing. The medical team will gradually transition you off the ventilator as you recover.
- Pain Management : You will receive pain medications from the surgical incision to manage discomfort and pain.
- Mobility : As soon as you're stable, the medical team will encourage you to start moving, turning, and sitting up to prevent complications like blood clots and improve lung function.
- Chest Tubes and Monitoring : Chest tubes may be inserted to drain excess fluid and air from around the heart and lungs. These are usually removed once drainage decreases and the lungs re-expand.
Days to Weeks After Surgery:
- Transition to Regular Hospital Room : Once stable, you will be transferred to a regular hospital room to continue your recovery.
- Physical Therapy : Physical therapists will help you gradually increase your activity level, regain strength, and improve mobility.
- Incision Care : Proper care of your incision is essential. Follow your medical team's instructions for wound care and hygiene to prevent infection.
- Diet : Your diet will be gradually advanced from liquids to solid foods. Nutritionists may guide postoperative dietary needs.
- Medications : You will be given drugs to manage pain, prevent infection, and support your heart's function. Follow the prescribed medication schedule.
Weeks to Months After Surgery:
- Continued Recovery at Home : Most patients are discharged from the hospital within a week, though the exact duration varies. Continue following your medical team's instructions for activity, wound care, and medication at home.
- Cardiac Rehabilitation : Your medical team may recommend a structured cardiac rehabilitation program to increase your physical activity under supervision gradually.
- Follow-up Appointments : Attend all scheduled follow-up appointments with your medical team to monitor your progress, assess the functioning of the new valve, and address any concerns.
- Return to Normal Activities : With time, you'll gradually be able to resume normal daily activities. The timing varies based on your progress and the type of activities.
- Emotional Well-being : Recovery can be emotionally challenging. Seek support from family, friends, or a counsellor if needed.
Long-Term Recovery:
- Medication Management : Some patients may need long-term medications to manage heart health and prevent complications.
- Lifestyle Changes : Follow your medical team's recommendations for maintaining a heart-healthy lifestyle, including a balanced diet, regular exercise, and avoiding smoking and excessive alcohol consumption.
- Follow-up Care : Regular follow-up appointments with your cardiologist are essential to monitor your heart health and the functioning of the replaced valve.
- Gradual Resumption of Activities : Over time, you'll be able to gradually resume more strenuous activities, as advised by your medical team.
Lifestyle Changes after Surgical Aortic Valve Replacement (SAVR) Procedure:
After undergoing Surgical Aortic Valve Replacement (SAVR), making specific lifestyle changes can contribute to a healthy recovery, improve your overall well-being, and support the long-term success of the procedure. Here are some lifestyle adjustments to consider:
- Heart-Healthy Diet:
- Consume a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Limit sodium intake to help manage blood pressure and reduce strain on the heart.
- Stay hydrated by drinking an adequate amount of water.
- Regular Physical Activity:
- Gradually engage in physical activity as recommended by your medical team. Start with light exercises and gradually increase intensity.
- Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, such as brisk walking, swimming, or cycling.
- Include strength training exercises to improve muscle tone and overall fitness.
- Medication Adherence:
- Take prescribed medications exactly as directed by your healthcare provider.
- If you're on blood thinners or other drugs, follow your medical team's guidelines to prevent complications.
- Tobacco and Alcohol:
- Quit smoking if you are a smoker, as smoking can negatively impact heart health and increase the risk of complications.
- Limit alcohol consumption and follow your medical team's recommendations.
- Stress Management:
- Practice relaxation techniques, meditation, deep breathing, or mindfulness to manage stress and promote emotional well-being.
- Engage in hobbies, spend time with loved ones, and pursue activities that bring you joy.
- Weight Management:
- Maintaining a healthy weight reduces the strain on your heart and improves cardiovascular health.
- Consult a dietitian for personalized guidance on portion control and weight management.
- Regular Follow-up Care:Attend all scheduled follow-up appointments with your cardiologist and medical team to monitor your heart health and the functioning of the replaced valve.
- Medication Management:Continue taking prescribed medications as your healthcare provider directs, even if you feel well.
- Dental Hygiene:Maintaining good oral hygiene reduces the risk of infections affecting overall health, including your heart.
- Listen to Your Body:Pay attention to your body's signals and seek prompt medical attention if you experience new or unusual symptoms.
- Sleep Health:Aim for 7-9 hours of sleep each night to support heart health and overall recovery.
- Support System:Lean on your support network of family and friends for emotional support and encouragement.
- Cardiac Rehabilitation:Participate in a structured cardiac rehabilitation program as recommended by your medical team. These programs offer supervised exercise and education on heart-healthy living.
- Limit Caffeine and Sugar:Reduce excessive caffeine and sugary foods, as they can affect blood pressure and heart health.