Best Pacemaker Implantation Surgery at Affordable Cost
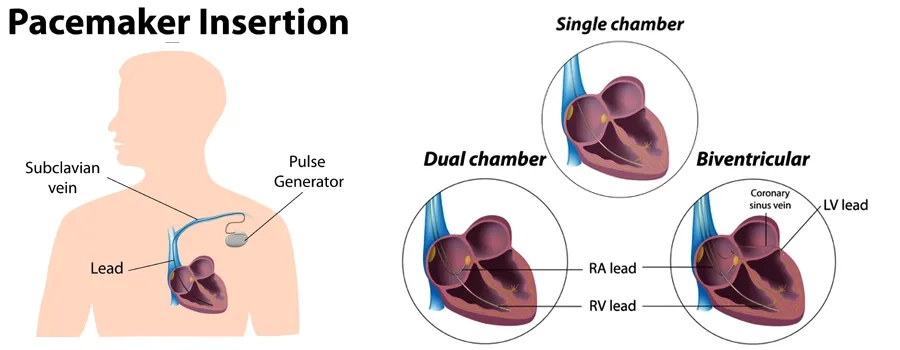
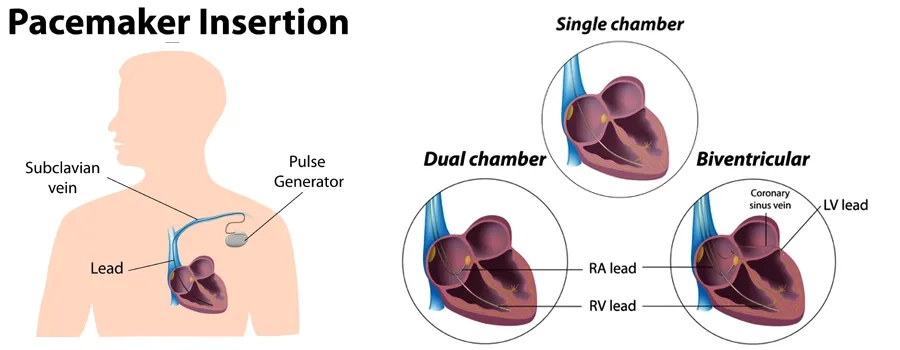
Pacemaker implantation surgery is a vital medical procedure designed to address irregular heart rhythms, known as arrhythmias, and restore the heart's natural rhythm. This surgical intervention involves the insertion of a small electronic device called a pacemaker, which acts as a guardian for the heart's electrical system. By generating controlled electrical impulses, the pacemaker ensures that the heart beats steadily and consistently, enhancing the overall well-being of individuals affected by abnormal heart rhythms.
Understanding Pacemaker Implantation Surgery:
The heart's rhythm is governed by electrical signals coordinating its contractions, ensuring efficient blood pumping throughout the body. However, disruptions in this electrical system can lead to irregular heartbeats, which may result in dizziness, fatigue, shortness of breath, and even fainting. Pacemaker implantation surgery aims to address these issues and provide patients with a reliable solution to maintain a healthy heart rhythm.
Steps involved in Pacemaker Implantation Surgery
Pacemaker Implantation Surgery: Procedure and Process
Pacemaker implantation surgery is a specialized procedure performed by cardiac electrophysiologists or cardiologists to address irregular heart rhythms (arrhythmias) and ensure a consistent heart rate. This surgery involves the insertion of a pacemaker, a small electronic device, to regulate the heart's electrical impulses and restore a normal rhythm. Here's an overview of what happens during a pacemaker implantation surgery:
-
Preoperative Preparations:
- You will receive instructions about fasting and medication adjustments before the surgery.
- An intravenous (IV) line might be placed to administer fluids and medications during the procedure.
- You'll be given anaesthesia to ensure you're comfortable and pain-free during the surgery.
-
Creating a Sterile Field:
- The surgical team will clean and sterilize the area where the pacemaker will be implanted, typically near the collarbone on the non-dominant side.
-
Incision and Pocket Creation:
- A small incision, usually about 2 to 3 inches long, is made beneath the skin to create a pocket for the pacemaker.
-
Lead Placement:
- Thin, insulated wires called leads are inserted through a vein and guided to the heart's chambers. These leads detect the heart's electrical signals and deliver impulses from the pacemaker.
-
Pacemaker Insertion:
- The pacemaker device is carefully inserted into the pocket beneath the skin. The leads are then connected to the pacemaker.
-
Testing and Programming:
- Once the pacemaker is in place, the surgical team tests its functionality to ensure proper lead positioning and pacing.
- The pacemaker's settings are customized to match your heart's needs. These settings can be adjusted later if necessary.
-
Closing the Incision:
- The incision is closed using sutures or surgical staples.
- A sterile dressing is applied to protect the incision site and prevent infection.
-
Postoperative Care:
- You'll be monitored as you wake up from anaesthesia.
- Depending on the procedure, you might need to spend a short time in a recovery area.
-
Recovery and Follow-Up:
- Most individuals can resume light activities within a few days, but strenuous exercises might be limited initially.
- You'll have follow-up appointments to monitor the pacemaker's function, adjust settings, and ensure proper healing.
Secure your health with a second opinion. Make informed decisions and book your appointment today!
Get A Second Opinion
Indications of Pacemaker Implantation
Pacemaker implantation Here are common indications for pacemaker implantation:
-
Bradycardia: Bradycardia refers to a slow heart rate, usually defined as a heart rate below 60 beats per minute. If bradycardia leads to dizziness, fainting, fatigue, or shortness of breath, a pacemaker may be necessary to ensure the heart maintains an appropriate rate.
-
Heart Block: Heart block is when the electrical signals between the heart's chambers are delayed or blocked, causing an irregular or slow heartbeat. If heart block leads to symptoms or negatively affects the heart's pumping ability, a pacemaker can help maintain a synchronized heartbeat.
-
Sick Sinus Syndrome: Sick sinus syndrome involves an irregular heartbeat caused by the heart's natural pacemaker (sinus node) dysfunction. A pacemaker can help regulate and restore a normal rhythm if the heart rate becomes too slow or inconsistent.
-
Tachy-Brady Syndrome: This condition involves alternating fast heartbeats (tachycardia) and slow heartbeats (bradycardia). A pacemaker can help stabilize the heart's rhythm.
-
Atrioventricular (AV) Block: AV block occurs when there is an interruption or delay in the electrical signals between the heart's upper (atria) and lower (ventricles) chambers. Depending on the severity, a pacemaker may be needed to ensure proper coordination between the atria and ventricles.
-
Heart Failure: In some cases of heart failure, a weakened heart muscle can lead to abnormal heart rhythms. A pacemaker, along with other treatments, may help improve heart function.
-
Syncope (Fainting) of Unknown Origin: If fainting episodes (syncope) are believed to be caused by bradycardia or other arrhythmias, a pacemaker might be recommended to prevent further attacks.
-
Long QT Syndrome: Long QT syndrome is an inherited disorder that can cause irregular heartbeats and fainting spells. In some cases, a pacemaker is used in conjunction with other treatments.
-
Recurrent Stokes-Adams Attacks: Stokes-Adams attacks are sudden loss of consciousness caused by a lack of blood flow to the brain due to abnormal heart rhythms. A pacemaker can prevent these episodes.
-
Symptomatic Arrhythmias: A pacemaker might be considered if other treatments fail to control symptomatic arrhythmias that significantly impact the patient's quality of life.
Who will treat for Pacemaker Implantation?
Medical Professionals Involved in Pacemaker Implantation and Treatment
Pacemaker implantation and treatment are typically managed by medical professionals specializing in cardiology and cardiac electrophysiology. These experts collaborate to evaluate, diagnose, and provide comprehensive care for individuals requiring pacemaker implantation. Here's an overview of the critical medical professionals involved:
-
Cardiologist: A cardiologist is a medical doctor who specializes in diagnosing and treating heart conditions. They play a central role in evaluating the need for pacemaker implantation based on the patient's medical history, symptoms, diagnostic tests, and overall cardiovascular health.
-
Cardiac Electrophysiologist: A cardiac electrophysiologist is a sub-specialist within cardiology who focuses on diagnosing and treating abnormal heart rhythms (arrhythmias). They have advanced training in understanding the heart's electrical system and are skilled in performing pacemaker implantation procedures.
-
Cardiothoracic Surgeon: A cardiothoracic surgeon may sometimes be involved, particularly if the pacemaker implantation is combined with other cardiac surgeries. They have expertise in surgical techniques and can collaborate with the electrophysiologist for more complex cases.
-
Anesthesiologist: An anesthesiologist is responsible for administering anaesthesia and ensuring the patient's comfort and safety during the procedure. They monitor the patient's vital signs and manage pain during the surgery.
-
Cardiac Nurses and Technicians: Nurses and technicians specializing in cardiac care provide critical support throughout the procedure. They assist with patient preparation, monitoring, and postoperative care.
-
Radiologic Technicians: Radiologic technicians operate imaging equipment, such as fluoroscopy or ultrasound, during the procedure to guide the placement of pacemaker leads and ensure accuracy.
Preparing for Pacemaker Implantation Surgery
Preparing for Pacemaker Implantation Surgery: Guidelines and Steps
Preparing for pacemaker implantation surgery involves several essential steps to ensure a smooth procedure and successful recovery. Here's a guide on how to prepare:
-
Consultation with Cardiologist: Schedule a consultation with your cardiologist or cardiac electrophysiologist. They will evaluate your medical history, symptoms, and diagnostic test results to determine if pacemaker implantation is necessary.
-
Medical Evaluation: Your medical team might perform additional tests, such as electrocardiogram (ECG), echocardiogram, and blood tests, to assess your heart's condition and overall health.
-
Medication Review: Inform your medical team about all medications you are taking, including prescription drugs, over-the-counter medications, and supplements. They will advise you on any medications you need to adjust before the surgery.
-
Fasting Instructions: Your medical team will provide instructions on fasting before the surgery. Typically, you'll be asked to avoid eating or drinking anything for several hours before the procedure.
-
Anesthesia Discussion: If anaesthesia will be administered, discuss any allergies, previous reactions, or concerns with the anesthesiologist.
-
Follow Instructions on Hygiene: Shower and wash your body with an antibacterial soap the night before or on the morning of the surgery. This helps reduce the risk of infection.
-
Stop Smoking: If you smoke, consider quitting or reducing Smoking before the surgery, as Smoking can affect healing.
-
Follow Preoperative Instructions: Your medical team will provide specific instructions about when to arrive, where to go, and what to expect on the day of the surgery.
Ready to take control of your health journey? Book your appointment now and start your path towards wellness today!
Book an Appointment
Recovery After Pacemaker Implantation Surgery
After undergoing pacemaker implantation surgery, recovery is necessary to allow the body to heal and adapt to the new device. Here's an overview of what you can expect during the recovery process:
-
Immediate Postoperative Period: After the surgery, you will be monitored in a recovery area while waking up from anaesthesia. Your heart's rhythm and vital signs will be closely observed to ensure the pacemaker functions correctly.
-
Hospital Stay: Most pacemaker implantations are outpatient, allowing you to go home the same day or within a short time after the surgery. In some cases, an overnight stay might be required for observation.
-
Incision Care: You will receive instructions on how to care for the incision site, including cleaning and changing dressings, to prevent infection.
-
Restrictions and Activity Guidelines: Your medical team will provide guidelines for physical activities during the initial recovery period. Strenuous activities, heavy lifting, and raising the arm on the side of the pacemaker might be restricted for a few weeks.
-
Medications: Your doctor might prescribe medications, including antibiotics and pain relievers, to manage pain and prevent infection.
-
Follow-Up Appointments: Regular follow-up appointments are crucial to monitor the pacemaker's function and ensure proper healing. Your medical team will adjust the pacemaker settings to optimize its performance.
-
Healing Process: The incision site will gradually heal over time. The sutures or staples used for closure might be removed during a follow-up appointment.
-
Resuming Daily Activities: You can usually resume light daily activities shortly after the surgery, but consult your medical team before engaging in more strenuous activities.
-
Pacemaker Use and Monitoring: Your medical team will provide instructions on using and caring for the pacemaker. The pacemaker will be programmed to your needs and monitored through regular check-ups.
Lifestyle changes after Pacemaker Implantation Surgery
After undergoing pacemaker implantation surgery, you can expect to make certain lifestyle adjustments to ensure the optimal function of your pacemaker and promote overall heart health. Here are some important considerations and lifestyle changes to keep in mind:
-
Medication Management: Follow your doctor's instructions regarding prescribed medications, especially those that might affect your heart rate or interact with your pacemaker.
-
Physical Activities: Most individuals can gradually resume light activities shortly after the surgery, but consult your medical team before engaging in more strenuous exercises or activities. Avoid activities that involve intense shoulder movement on the side of the pacemaker for a few weeks.
-
Hydration and Nutrition: Maintain a balanced and heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. Stay adequately hydrated, as dehydration can impact heart function.
-
Smoking and Alcohol: If you smoke, consider quitting or reducing Smoking, as Smoking can adversely affect heart health. Consume alcohol in moderation, as excessive alcohol consumption can adversely affect the heart.
-
Stress Management: Practice stress-relief techniques such as deep breathing, meditation, yoga, or engaging in hobbies you enjoy.
-
Medical Follow-Up: Attend all scheduled follow-up appointments to monitor the pacemaker's function and adjust settings if necessary.
-
Device Identification: Carry a card in your wallet or wear a medical alert bracelet indicating that you have a pacemaker. This is important in case of emergencies.
-
Electromagnetic Interference: Be cautious around devices that emit strong electromagnetic fields, such as giant magnets, MRI machines, and specific electronic equipment. Consult your medical team for guidance.
-
Dental Procedures: Inform your dentist about your pacemaker before dental procedures, as some equipment might interfere with the device.
-
Travel and Security Screening: Inform airport security personnel about your pacemaker before going through metal detectors. It's unlikely to affect the pacemaker but inform them for your peace of mind.
-
Regular Check-Ups: Continue routine check-ups with your cardiologist or cardiac electrophysiologist to monitor your heart health and pacemaker function.