Hemodialysis: Overview
Hemodialysis surgery is a crucial medical procedure that assists individuals with compromised kidney function. When the kidneys struggle to filter waste and excess fluids from the blood, hemodialysis steps in as a lifeline. During the procedure, blood is redirected through a dialysis machine, where it is cleansed of toxins and returned to the body.
Steps involved in Hemodialysis Procedure
The AV hemodialysis procedure, also known as arteriovenous hemodialysis, involves creating an arteriovenous fistula (AV fistula) to provide a reliable access point for hemodialysis treatments. Here's what happens during the AV hemodialysis procedure:
- Patient Evaluation: Before the procedure, a thorough evaluation of the patient's vascular anatomy is conducted. This helps determine the suitability of the arteries and veins for creating the AV fistula.
- Anesthesia: Local anesthesia is administered to numb the area where the AV fistula will be created. This ensures that the patient remains comfortable throughout the procedure.
- AV Fistula Creation:
- The surgeon makes an incision over the chosen artery and vein, typically in the arm.
- The artery and vein are carefully exposed, and the surgeon creates an opening in both vessels.
- The artery and vein are then directly connected, either through sutures or a synthetic graft, creating the AV fistula.
- Blood Flow Check: After creating the AV fistula, the surgeon checks the blood flow to ensure proper circulation through the newly created connection.
- Maturation Period: Following the procedure, the AV fistula needs time to "mature." During this period, the vein gradually thickens and strengthens, making it suitable for repeated needle insertions during hemodialysis.
- Hemodialysis Access:
- Once the AV fistula is mature, it serves as an access point for hemodialysis treatments.
- During hemodialysis sessions, two needles are inserted into the fistula—one to draw blood from the body into the dialysis machine, and the other to return clean blood from the machine to the body.
- Ongoing Care: Regular follow-up appointments with healthcare professionals are essential to monitor the AV fistula's function and address any issues that may arise.
Who will Treat for Hemodialysis Procedure
To undergo hemodialysis surgery, you would need to connect with a healthcare team that specializes in kidney care and dialysis. Here's whom you would typically contact for hemodialysis surgery:
- Nephrologist: A nephrologist is a medical doctor who specializes in kidney health. They will assess your kidney function, determine the need for hemodialysis, and provide guidance on the appropriate treatment plan.
- Dialysis Center: Dialysis centers are specialized facilities equipped to provide various types of dialysis treatments, including hemodialysis. Contacting a dialysis center is a common way to access hemodialysis surgery.
- Nephrology Department of a Hospital: Many hospitals have dedicated nephrology departments where you can consult with nephrologists and receive information about hemodialysis surgery.
- Primary Care Physician: Your primary care physician can provide referrals to nephrologists or dialysis centers for further evaluation and guidance.
- Medical Referrals: You can ask your primary care physician or other healthcare providers for recommendations and referrals to specialists who can perform hemodialysis surgery.
- Internet Research: You can research dialysis centers, hospitals, and nephrology specialists online to find facilities or experts specializing in hemodialysis.
- Healthcare Insurance Provider: If you have health insurance, your insurance provider can guide you to healthcare facilities and professionals within their network who offer hemodialysis services.
- Local Support Groups: Support groups for individuals with kidney conditions may provide valuable information about local resources and healthcare providers specializing in hemodialysis.
Preparing for Hemodialysis Surgery
Preparing for hemodialysis surgery involves several important steps to ensure that you are physically and mentally ready for the procedure. Here's a guide on how to prepare:
- Consultation with Nephrologist: Start by consulting with a nephrologist (kidney specialist) to determine the need for hemodialysis and discuss the procedure.
- Medical Evaluation: Undergo a comprehensive medical evaluation to assess your overall health and suitability for hemodialysis.
- Understand the Procedure: Learn about the hemodialysis procedure, its purpose, the process involved, and what to expect before, during, and after the surgery.
- Share Medical History: Provide your healthcare team with a detailed medical history, including past surgeries, medical conditions, allergies, and medications you are taking.
- Medication Review: Inform your healthcare team about all medications, supplements, and herbal remedies you are taking. Some medications may need to be adjusted before the surgery.
- Blood Tests: Complete any necessary blood tests to assess your kidney function, blood clotting ability, and overall health.
- Fasting Instructions: Follow any fasting instructions provided by your healthcare team. You may need to avoid food and liquids for a specified period before the surgery.
- Hydration: Stay adequately hydrated in the days leading up to the surgery. Proper hydration supports your body's healing process.
- Stop Smoking: If you smoke, consider quitting or at least refraining from smoking before and after the surgery. Smoking can impact healing and increase the risk of complications.
- Arrange Transportation: Plan for transportation to and from the surgical facility, as you might not be able to drive immediately after the procedure due to anesthesia.
- Arrange Support: Enlist a family member or friend to provide support during your recovery period.
- Mental Preparation: Prepare yourself mentally for the surgery. Understand the benefits of hemodialysis and the role it plays in improving your health.
- Preoperative Instructions: Follow any preoperative instructions provided by your healthcare team, including guidelines on medication intake and bathing before the surgery.
- Communication: Keep an open line of communication with your healthcare team. Address any concerns or questions you may have before the surgery.
During a typical hemodialysis treatment session
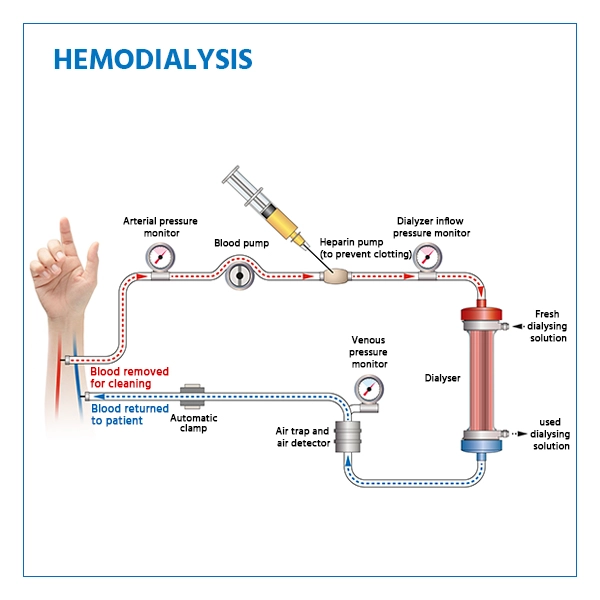
- Vascular Access: Before hemodialysis can begin, a suitable vascular access point is established. This can be done through an arteriovenous fistula (AV fistula), arteriovenous graft (AV graft), or central venous catheter. The access point allows blood to be safely withdrawn from the body and returned after dialysis.
- Preparing the Access Point: If you have an AV fistula or AV graft, the dialysis team will insert two needles into the access site. One needle draws blood from your body into the dialysis machine, and the other returns cleaned blood to your body.
- Connection to Dialysis Machine: The needles are connected to tubes that lead to the dialysis machine. The machine contains a special filter called a dialyzer that mimics the kidney's function of filtering toxins and excess fluids from the blood.
- Blood Filtration: Blood flows into the dialyzer, and on the other side of the dialyzer, a sterile solution called dialysate helps draw out waste and excess fluids from the blood.
- Monitoring and Adjustments: During the hemodialysis session, your vital signs are closely monitored, and the dialysis machine is adjusted as needed to ensure a safe and effective treatment.
- Duration of Treatment: A typical hemodialysis treatment session lasts about 3 to 4 hours, and it can vary based on individual needs and the prescribed treatment plan.
- Completion of Treatment: Once the treatment is complete, the cleaned blood is returned to your body, and the needles are removed from the access site.
- Post-Dialysis Care: After the treatment, the access site is cleaned and dressed to prevent infection. You can resume your regular activities after a brief rest.
Recovery after Hemodialysis Procedure
- Post-Dialysis Fatigue: Some patients may experience fatigue after a hemodialysis session due to the physical demands of the treatment. This is normal and usually improves over time.
- Dietary Considerations: Following a specific diet recommended by your healthcare team is crucial to ensure that your body's nutritional balance is maintained between dialysis sessions.
- Fluid Intake Management: It's important to monitor your fluid intake between dialysis sessions, as excessive fluid intake can lead to fluid overload and potential complications.
- Medication Management: If you're taking medications, it's important to coordinate their administration with your healthcare team, as some medications might need to be adjusted based on your dialysis schedule.
- Lifestyle Adjustments: Adapting to the hemodialysis schedule may require adjustments to your daily routine, especially considering the time and energy spent during dialysis sessions.
- Emotional Well-being: Managing a chronic condition like kidney failure and undergoing regular hemodialysis can impact your emotional well-being. It's important to seek support and engage in activities that bring you joy.
Lifestyle changes after Hemodialysis Procedure
- Dietary Restrictions: Follow a specific diet plan recommended by your healthcare team. This may involve limiting sodium, potassium, phosphorus, and fluid intake to help manage electrolyte balance and fluid levels.
- Fluid Intake Management: Monitor your fluid intake closely, as excessive fluid consumption can lead to fluid overload and strain on the heart.
- Medication Adherence: Take prescribed medications as directed by your healthcare provider. These medications can help manage blood pressure, anemia, and other conditions associated with kidney disease.
- Regular Medical Appointments: Attend all scheduled medical appointments with your nephrologist, healthcare team, and dialysis center. Regular check-ups are essential to monitor your condition and adjust your treatment plan as needed.
- Physical Activity: Engage in regular physical activity as advised by your healthcare provider. Staying active can help improve circulation, maintain muscle strength, and support overall well-being.
- Stress Management: Practice stress-reducing techniques such as meditation, deep breathing, or yoga to help manage stress and promote emotional well-being.
- Avoid Smoking and Alcohol: If you smoke, quitting is highly recommended, as smoking can worsen kidney function. Limit or avoid alcohol consumption as well.
- Skin and Access Care: If you have a vascular access site for hemodialysis, take proper care of it to prevent infections and complications.
- Dental Care: Maintain good oral hygiene to prevent infections that could affect your overall health.
- Get Vaccinated: Stay up to date with vaccinations, including flu and pneumonia vaccines, to protect your immune system.
- Monitor Blood Pressure: Regularly monitor your blood pressure and take any prescribed medications to control it. High blood pressure can further damage kidneys.
- Education and Self-Care: Learn about your condition and treatment. Engage in self-care practices to better manage your health.
- Limit High-Potassium Foods: Consume fewer high-potassium foods like bananas, oranges, tomatoes, and potatoes to help control potassium levels.
- Limit High-Phosphorus Foods: Reduce intake of high-phosphorus foods like dairy products, processed meats, and certain beans to manage phosphorus levels.
- Protein Intake: Adjust your protein intake based on your healthcare provider's recommendations to help manage waste buildup.