There are generally two main approaches to breast reconstruction:
- Implant-Based Reconstruction: In this approach, a breast implant is used to recreate the breast mound. The surgeon may place the implant either beneath the chest muscle (subpectoral) or on top of the muscle and beneath the remaining breast tissue (subcutaneous). The implant has the option to be filled with either saline or silicone gel. This technique is often chosen when the patient desires a quicker recovery time and has sufficient tissue coverage to support the implant.
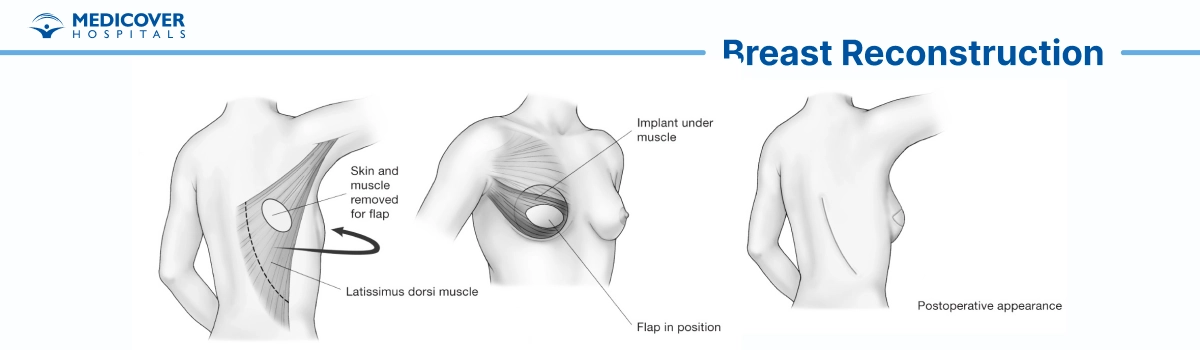
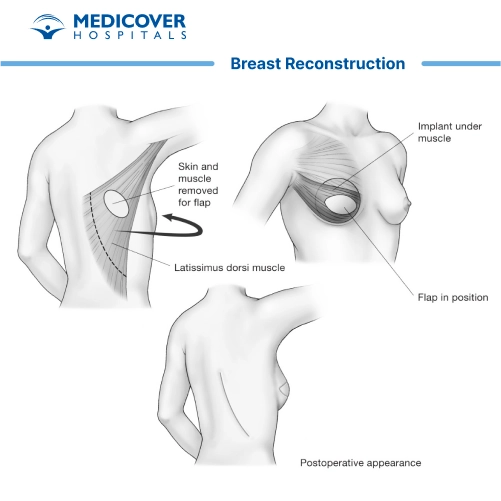
- Autologous Tissue (Flap) Reconstruction: Autologous tissue reconstruction involves using the patient's own tissue, usually taken from areas like the abdomen, buttocks, or thigh, to reconstruct the breast. The most common type of autologous reconstruction is the TRAM (transverse rectus abdominis myocutaneous) flap, which utilizes abdominal tissue. Other flap techniques include the DIEP (deep inferior epigastric perforator) flap and the latissimus dorsi flap. This approach is often chosen when there is inadequate tissue coverage or when the patient prefers a more natural-feeling breast.
Indications of Breast Reconstruction Surgery:
Breast reconstruction surgery is recommended for individuals who have undergone mastectomy (complete or partial removal of one or both breasts) or have experienced significant breast tissue loss due to various reasons. The primary indications and purposes of breast reconstruction surgery include:
- Breast Cancer Treatment: Breast reconstruction is often a crucial part of the comprehensive treatment plan for breast cancer patients who have undergone mastectomy. It helps restore the physical appearance of the breasts, contributing to the overall well-being and quality of life of these individuals. Reconstruction can also aid in emotional healing and recovery by helping patients regain a sense of normalcy after cancer treatment.
- Traumatic Injury or Accidents: Women who have experienced traumatic injuries or accidents that result in substantial breast tissue loss may opt for breast reconstruction to restore the appearance of the affected breast. This can significantly improve self-esteem and body image, leading to better psychological and emotional outcomes.
- Congenital Deformities or Developmental Issues: Some individuals are born with congenital breast deformities or experience developmental issues that result in asymmetry or underdeveloped breasts. Breast reconstruction can address these concerns and create a more balanced and harmonious breast appearance.
- Prophylactic Mastectomy: Women with a high risk of developing breast cancer, often linked to genetic mutations like BRCA1 or BRCA2, or a notable family history of the disease, might opt for a proactive approach. This entails undergoing a preventive mastectomy, a surgical procedure involving the removal of breast tissue to reduce the likelihood of future cancer development. Breast reconstruction has the flexibility to be carried out either directly after a mastectomy or in the future, strategically mitigating the chances of breast cancer while preserving an aesthetically pleasing breast contour.
- Improved Body Symmetry: For some women, breast reconstruction is desired to achieve or restore body symmetry. This can be particularly relevant for those who want to achieve a more balanced overall appearance, especially when only one breast has been affected by surgery or trauma.
- Enhanced Psychological and Emotional Well-Being: Breast reconstruction surgery can have a profound impact on a person's self-esteem, self-confidence, and emotional well-being. Restoring a natural-looking breast can help individuals feel more comfortable in their bodies and improve their overall quality of life.
- Aesthetic Preferences: Some women choose breast reconstruction purely for aesthetic reasons, desiring a more symmetrical and pleasing breast appearance. While medical necessity often underlies the decision, aesthetic considerations can also play a role in the choice to undergo breast reconstruction.
Steps involved in Breast Reconstruction Surgery:
Breast reconstruction surgery is a multi-step process that involves careful planning, precise surgical techniques, and coordination between different medical professionals. The exact procedure can vary based on the chosen reconstruction technique, whether implant-based or autologous tissue reconstruction. Here's an overview of what generally happens during breast reconstruction surgery:
- Anesthesia: The surgery typically begins with the administration of anesthesia, which ensures that you are comfortable and pain-free throughout the procedure. The type of anesthesia used (general or local with sedation) will be discussed and determined during your preoperative consultations.
- Incision and Tissue Preparation: Depending on the chosen technique, the plastic surgeon will make incisions in the appropriate areas. For implant-based reconstruction, incisions may be made in the breast crease, around the areola, or in the underarm area. For autologous tissue reconstruction, tissue from donor sites (such as the abdomen, buttocks, or thigh) will be carefully harvested and prepared.
- Implant Placement or Tissue Reconstruction: If you're undergoing implant-based reconstruction, the surgeon will create a pocket in the breast area and insert the chosen implant (filled with saline or silicone gel). If you're having autologous tissue reconstruction, the harvested tissue will be shaped and placed in the breast area to create a natural-looking breast mound.
- Nipple and Areola Reconstruction (Optional): In some cases, nipple and areola reconstruction may be performed during the same surgery or in a subsequent procedure. This involves creating a nipple mound and adding pigmentation to mimic the appearance of a natural nipple and areola.
- Closure and Dressings: After achieving the desired breast shape and symmetry, the surgeon will carefully close the incisions using sutures or other closure techniques. Dressings and surgical tape may be applied to protect the incision sites and promote healing.
- Drains (if necessary): Depending on the surgical technique and your individual case, temporary drainage tubes (drains) may be placed to remove excess fluid from the surgical site. These drains help reduce the risk of fluid accumulation and promote proper healing.
- Recovery and Monitoring: Following the procedure, you'll be transferred to a designated recovery zone where vigilant observation will be maintained as you gradually emerge from anesthesia. Medical personnel will carefully track your essential signs and administer pain relief as needed to alleviate any discomfort.
- Hospital Stay (if applicable): The length of your hospital stay will depend on the complexity of the procedure, your overall health, and the surgical approach used. Some patients may go home on the same day, while others may require a short hospital stay.
- Postoperative Care: You will receive detailed postoperative instructions from your surgical team. These instructions will cover wound care, activity restrictions, and any necessary follow-up appointments.
Who will do Breast Reconstruction Surgery:
Breast reconstruction surgery is a specialized procedure that involves a team of healthcare specialists working together to ensure the best possible outcome for the patient. Breast reconstruction surgery involves a collaborative team of specialists:
- Breast Surgeon: Performs mastectomy and coordinates the reconstruction plan.
- Plastic Surgeon: Reconstructs the breast using various techniques like implants or tissue flaps.
- Oncologist: Oncology specialist Advises on reconstruction timing in cancer cases.
- Anesthesiologist: Administers anesthesia and monitors vital signs.
- Nurse Navigator: Guides patients through the process and appointments.
- Psychologist/Counselor: Provides emotional support.
- Physical Therapist: Aids in post-surgery recovery.
- Supportive Care Team: Includes nutritionists, social workers, and support groups.
Preparation for Breast Reconstruction Surgery:
Preparing for breast reconstruction surgery involves careful planning and coordination with your medical team. Here are some steps to help you get ready for the procedure:
- Consultation with Plastic Surgeon: Book an appointment with a breast reconstruction surgery specialist who specializes in breast reconstruction. Discuss your goals, medical history, and preferences. Your surgeon will assess your individual case and recommend the most suitable reconstruction options.
- Medical Evaluation: Undergo a thorough medical assessment to ensure you are in good health for surgery. This may include blood tests, imaging, and other tests as needed.
- Quit Smoking and Alcohol: If you smoke or consume alcohol, consider quitting or reducing these habits before surgery. Smoking can impair healing, and alcohol can interfere with anesthesia and medication.
- Medication Review: Inform your medical team about all medications, supplements, and herbal remedies you are taking. Some medications may need to be adjusted before surgery.
- Healthy Lifestyle: Prioritize a healthy diet and exercise routine to optimize your overall health and support your body's healing process.
- Manage Chronic Conditions: In case you have ongoing health conditions like diabetes or hypertension, it's advisable to collaborate closely with your medical professional to effectively regulate and stabilize these conditions before undergoing surgery.
- Arrange Support: Plan for someone to assist you with daily activities during your recovery, especially in the initial days after surgery.
- Preoperative Instructions: Follow any preoperative instructions provided by your surgical team, such as fasting before surgery and avoiding certain medications.
- Emotional Preparation: Consider seeking emotional support from counselors, support groups, or friends and family. Breast reconstruction can have a significant emotional impact, and being mentally prepared is important.
- Logistics: Arrange transportation to and from the hospital or surgical facility on the day of surgery. Make sure you have comfortable clothing to wear post-surgery.
- Postoperative Recovery Area: Set up a comfortable recovery area at home with pillows, blankets, and any necessary supplies.
- Communication with Employer: Communicate with your employer about your upcoming surgery and discuss any necessary time off for recovery.
- Follow Fasting Instructions: Adhere to fasting instructions provided by your surgical team to ensure a safe surgery and anesthesia administration.
- Pack Essentials: If you need to stay overnight, pack essentials such as toiletries, comfortable clothing, and personal items.
- Ask Questions: Don't hesitate to ask your surgical team any questions you may have about the procedure, recovery, and potential risks.
Recovery After Breast Reconstruction Surgery:
Recovery after breast reconstruction surgery is a gradual process that requires patience, proper care, and adherence to your medical team's instructions. The duration and specific steps of recovery can vary depending on the surgical technique used, your overall health, and individual factors. Here are some general guidelines for the recovery period:
Immediate Postoperative Period:
- Hospital Stay (if applicable): Depending on the type of reconstruction and your surgeon's recommendations, you may spend a night or more in the hospital for observation and initial recovery.
- Pain Management: Pain and discomfort are common after surgery. Your medical team will provide pain medication to help manage any discomfort. Take medications as prescribed and inform your healthcare provider if you experience severe or unusual pain.
- Monitoring and Care: Medical staff will monitor your condition, including vital signs and surgical sites, during your hospital stay.
Recovery at Home:
- Follow Instructions: Adhere to the postoperative instructions provided by your surgical team. This includes wound care, dressing changes, and any activity restrictions.
- Rest and Activity: Ensure ample rest during the initial weeks, allowing your body time to recuperate. Gradually escalate your engagement in activities according to the guidance provided by your healthcare professionals. Refrain from engaging in demanding tasks or lifting heavy objects during the initial phase of recovery.
- Drains (if applicable): If drains were placed during surgery, follow instructions for caring for them, and record drainage amounts as instructed. Drains are typically removed once fluid output decreases.
- Medications: Take prescribed medications as directed, including any antibiotics or pain relievers. Avoid over-the-counter medications unless approved by your surgeon.
- Compression Garments (if applicable): If instructed, wear any compression garments or surgical bras as recommended to support healing and reduce swelling.
- Diet and Hydration: Maintain a healthy diet and stay hydrated to support healing and overall well-being.
- Wound Care: Keep surgical incisions clean and dry. Follow guidelines for changing dressings and caring for incision sites to prevent infection.
- Follow-Up Appointments: Attend all scheduled follow-up appointments with your surgical team. These appointments are crucial for monitoring your progress and addressing any concerns.
Long-Term Recovery:
- Scar Management: As scars heal, follow your surgeon's recommendations for scar care, which may include the use of scar creams or silicone sheets.
- Physical Therapy (if applicable): If you underwent autologous tissue reconstruction, physical therapy may be recommended to aid in regaining strength and mobility.
- Emotional Well-Being: Focus on your emotional recovery as well. Reach out to counselors, support groups, or mental health professionals if needed.
- Return to Normal Activities: Gradually resume normal activities as advised by your medical team. Return to work and exercise routines based on their guidance.
Lifestyle Changes after Breast Reconstruction Surgery:
After undergoing breast reconstruction surgery, there are certain lifestyle adjustments that can help promote healing, enhance your overall well-being, and ensure the best possible outcomes. Here are some lifestyle changes and considerations to keep in mind during your recovery and beyond:
- Follow Medical Instructions: Adhere to all postoperative instructions provided by your surgical team. This includes wound care, medication management, and any activity restrictions. Following these guidelines is essential for a smooth recovery.
- Balanced Diet and Hydration: Maintain a nutritious diet rich in vitamins, minerals, and protein to support your body's healing process. Stay hydrated by drinking plenty of water. Proper nutrition can enhance your immune system and aid in recovery.
- Quit Smoking and Limit Alcohol: If you smoke, consider quitting, as smoking can impair healing and increase the risk of complications. Limit alcohol consumption, as it can interfere with medication and the healing process.
- Physical Activity: Gradually resume physical activity as approved by your medical team. Engage in light exercise and activities to promote circulation, reduce the risk of blood clots, and support your overall well-being. Consult your surgeon before returning to more strenuous activities.
- Supportive Bras: Wear supportive bras that provide adequate support and comfort for your healing breasts. Your surgical team can recommend appropriate bras or compression garments based on your specific needs.
- Scar Care: Follow your surgeon's instructions for scar care, which may include applying scar creams or silicone sheets. Protect scars from sun exposure to prevent hyperpigmentation.
- Emotional Well-Being: Focus on your emotional recovery as well. Engage in activities that promote relaxation and reduce stress. Consider joining support groups or seeking counseling if needed.
- Regular Check-Ups: Maintain regular follow-up appointments with your surgical team to monitor your progress, address any concerns, and ensure proper healing.
- Clothing Choices: Experiment with clothing styles that help you feel comfortable and confident. Different necklines and clothing cuts can help you feel more at ease and showcase your new breast appearance.
- Body Positivity and Self-Care: Embrace a positive body image and practice self-care. Engage in activities that boost your self-esteem and help you feel good about your body.
- Sun Protection: Protect your scars from sun exposure by using sunscreen or wearing protective clothing. Sun can cause scars to darken and become more noticeable.
- Counseling and Support Groups: Consider participating in counseling or joining support groups for individuals who have undergone breast reconstruction. Connecting with others who have shared similar experiences can provide emotional support and a sense of community.