Indications of Anterior Colporrhaphy:
Anterior colporrhaphy is a surgical procedure that serves a specific set of indications and purposes, primarily focused on addressing anterior vaginal wall prolapse, also known as cystocele.
- Anterior Vaginal Wall Prolapse (Cystocele): The most common indication for anterior colporrhaphy is the presence of anterior vaginal wall prolapse, also known as cystocele. This occurs when the bladder descends and protrudes into the vaginal canal due to weakened or stretched pelvic floor muscles and ligaments.
- Pelvic Pressure and Discomfort: Women experiencing symptoms of pelvic pressure, fullness, or discomfort, especially when standing, walking, or engaging in physical activities, may be candidates for anterior colporrhaphy.
- Urinary Incontinence: If anterior vaginal wall prolapse contributes to urinary incontinence (leakage of urine during coughing, sneezing, laughing, or physical activity), anterior colporrhaphy can help address this issue by restoring proper bladder positioning and support.
- Visible Bulging or Prolapse: When the bladder bulges into the vaginal canal and causes a noticeable bulge or protrusion, this may be an indication for anterior colporrhaphy. Visible prolapse is often a significant concern for patients and may lead to discomfort and reduced quality of life.
- Challenges During Intercourse: Anterior vaginal wall prolapse can leads to discomfort or pain during sexual intercourse (dyspareunia) due to the pressure on the vaginal canal. Women experiencing sexual dysfunction related to prolapse may benefit from anterior colporrhaphy.
- Failed Conservative Management: If non-surgical interventions such as pelvic floor exercises, pessaries, or lifestyle modifications have not provided adequate relief from anterior vaginal wall prolapse and its associated symptoms, anterior colporrhaphy may be considered as a more definitive treatment option.
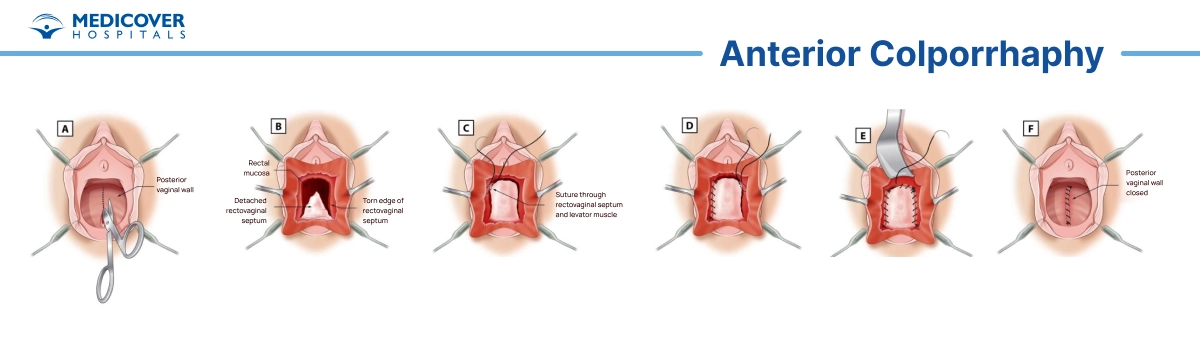
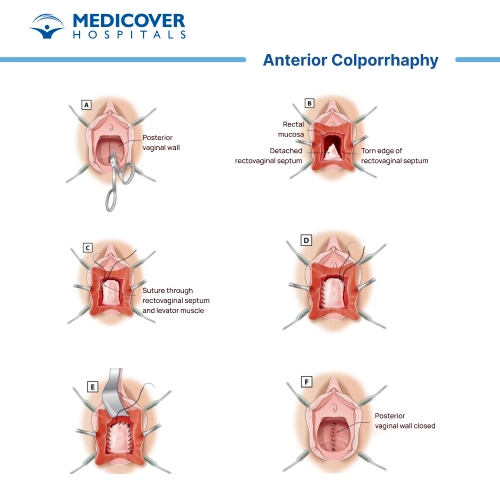
Steps involved in Anterior colporrhaphy
Anterior colporrhaphy is a surgical procedure performed to correct a condition called cystocele or anterior vaginal wall prolapse, where the bladder bulges into the front wall of the vagina. The procedure involves repairing and reinforcing the tissues of the anterior vaginal wall to provide support to the bladder. Here are the general steps involved in an anterior colporrhaphy
- Preoperative Preparation: The patient undergoes a medical evaluation, including a physical examination and sometimes imaging tests, to assess the extent of the cystocele and ensure they are a suitable candidate for the surgery.
- Consent and Anesthesia:
- The patient meets with the surgeon to discuss the procedure, its benefits, risks, and potential alternatives. Informed consent is obtained.
- Anesthesia is administered to ensure the patient is comfortable and pain-free during the surgery. General anesthesia or regional anesthesia (such as epidural or spinal anesthesia) may be used.
- Positioning: The patient is positioned on the operating table in a lithotomy position, with their legs placed in stirrups. This provides optimal access to the surgical area.
- Preparation of the Surgical Site: The genital area is cleansed and sterilized to reduce the risk of infection.
- Incision: An incision is made in the vaginal wall near the front wall (anterior) of the vagina. The size and location of the incision may vary based on the surgeon's technique and the extent of the prolapse.
- Exposure of the Cystocele: The surgeon gently retracts the vaginal tissues to expose the underlying bladder and the weakened or damaged tissues causing the cystocele.
- Tissue Repair and Reinforcement:
- The weakened tissues are repaired and reinforced to provide support to the bladder and correct the prolapse.
- The surgeon might use sutures or other specialized techniques to tighten and reposition the tissues.
- Closure: After the repair is complete, the vaginal incision is closed using absorbable sutures or stitches that will dissolve over time.
- Recovery and Observation: The patient is taken to a recovery area as they wake up from anesthesia. Vital signs are monitored, and pain management measures are implemented.
- Hospital Stay: Most anterior colporrhaphy procedures are done on an outpatient basis, allowing patients to return home the same day. In some cases, a short hospital stay may be required.
- Postoperative Care: Patients receive instructions for wound care, pain management, and activities to avoid during the recovery period.
- Follow-Up Appointments: Follow-up appointments are scheduled to monitor the healing process, assess the success of the repair, and address any concerns.
Who will Treat for Anterior Colporrhaphy
For individuals considering anterior colporrhaphy, it's important to seek care from qualified and experienced healthcare professionals who specialize in gynecology, urogynecology, or pelvic floor disorders. Here are the types of healthcare providers you may contact and consult with regarding anterior colporrhaphy:
- Gynecologist: Gynecologists are medical doctors who specialize in women's reproductive health, including the diagnosis and treatment of conditions affecting the female reproductive system. They are well-equipped to evaluate and manage anterior vaginal wall prolapse and can provide recommendations for surgical interventions like anterior colporrhaphy if necessary.
- Urogynecologist: Urogynecologists are specialists who focus on the evaluation and treatment of pelvic floor disorders, including prolapse and urinary incontinence. They have advanced training in both gynecology and urology and are highly skilled in managing complex pelvic floor conditions. Urogynecologists are well-suited to provide comprehensive care and perform anterior colporrhaphy procedures.
- Pelvic Floor Specialist: Some healthcare centers may have specialists who specifically focus on pelvic floor disorders, including anterior vaginal wall prolapse. These specialists may include pelvic physical therapists or nurse practitioners with expertise in pelvic health. They can offer non-surgical treatment options, provide guidance on pelvic floor exercises, and refer you to a surgeon if surgery is indicated.
- Medical Team: In some cases, a team approach may be taken, involving various healthcare providers working together to provide comprehensive care. This team may include gynecologists, urogynecologists, colorectal surgeons (if needed for concurrent conditions), nurses, and physical therapists. Collaboration among these professionals ensures that you receive well-rounded and personalized care.
Preparing for the surgery?
Preparing for anterior colporrhaphy surgery involves several important steps to ensure a safe, secure & successful procedure, as well as a smooth recovery. Here's a general guide on how to prepare:
- Consultation and Evaluation:
- Schedule a consultation with your chosen healthcare provider, such as a gynecologist, urogynecologist, or pelvic floor specialist.
- Discuss your symptoms, medical history, current medications, and any allergies you have.
- Be open about your expectations and concerns regarding the surgery.
- Preoperative Testing: Your healthcare provider may order certain tests, such as blood tests, urinalysis, and possibly imaging (ultrasound or MRI), to assess your overall health and help plan the surgery.
- Medications:
- Follow your healthcare provider's instructions regarding medications. You may need to adjust or temporarily stop taking some medications, especially those that can increase bleeding or interact with anesthesia.
- Inform your healthcare provider about any over-the-counter supplements or herbal remedies you're taking, as they may also impact the surgery.
- Smoking and Alcohol:
- If you smoke, try to quit or at least reduce smoking before surgery, as smoking can affect the wound healing and increase the risk of complications.
- Avoid alcohol consumption in the days leading up to the surgery, as it can interfere with anesthesia and recovery.
- Nutrition and Hydration:
- Maintain a proper balanced diet rich in vitamins and nutrients to support your body's healing process.
- Ensure you maintain proper hydration by consuming an ample amount of water, as it contributes to a more effective recovery process.
- Preoperative Instructions: Follow any specific preoperative instructions provided by your healthcare provider. This may include guidelines on fasting before surgery (usually no food or drink after midnight the night before).
- Arrangements for Surgery Day:
- Arrange for transportation to and from the hospital or surgical center, as you will likely be unable to drive after the surgery.
- Ensure you have someone available to help you at home during the initial recovery period.
- Personal Care:
- Take care of personal hygiene, including bathing or showering before the surgery.
- Remove any nail polish and makeup, as well as jewelry, before the surgery.
- Clothing and Comfort:
- Wear loose, comfortable clothing on the day of the surgery.
- Leave valuables and excess belongings at home.
- Mental and Emotional Preparation:
- Address any anxiety or concerns you may have about the surgery by discussing them with your healthcare provider.
- Engage in relaxation techniques, meditation, or other stress-reducing activities.
- Questions and Clarifications: Make a list of questions to ask your healthcare provider during your preoperative appointment. It's important to have a clear understanding of the procedure, recovery process, and potential risks.
- Health Insurance and Financial Considerations: Verify your health insurance coverage and any financial responsibilities associated with the surgery.
Recovery after Anterior Colporrhaphy Surgery
Recovery after anterior colporrhaphy surgery is a crucial period during which your body heals and adjusts to the changes made during the procedure. It's important to follow your healthcare provider's postoperative instructions carefully to ensure a smooth and successful recovery.
Immediate Postoperative Period:
- Hospital Stay: Most patients are discharged on the same day as the surgery or after a short hospital stay, depending on the surgeon's preference and your individual circumstances.
- Pain Management: You may experience some discomfort or pain at the surgical site. Your healthcare provider will prescribe pain medication to help manage any discomfort.
- Vaginal Packing: If your surgeon used gauze to pack the vaginal canal during surgery, it will typically be removed within the first day or two after surgery.
- Catheter: In some cases, a temporary urinary catheter may be placed to assist with bladder emptying. It will be removed once you are able to urinate comfortably on your own.
First Few Weeks:
Activity Restrictions: Your healthcare provider will provide guidelines on physical activity and lifting restrictions. You may need to avoid heavy lifting, strenuous exercise, and sexual activity for a specified period to allow the surgical site to heal.
Pain and Discomfort: Some pain, swelling, and discomfort are normal during the initial weeks. Use prescribed pain medication as directed and report any unusual or severe symptoms to your healthcare provider.
Hygiene: Follow your healthcare provider's instructions for proper hygiene and wound care. You may need to avoid soaking in baths and using tampons during the initial recovery period.
Long-Term Recovery:
- Follow-Up Appointments: It is important to attend all scheduled follow-up appointments with your healthcare specialist as they are essential for monitoring your progress and addressing any concerns
- Resuming Activities: As you heal, you'll gradually be able to resume normal activities based on your healthcare provider's guidance. It's important to listen to your body and avoid pushing yourself too quickly.
- Pelvic Floor Exercises: Your healthcare provider may recommend pelvic floor exercises (Kegels) to help strengthen the pelvic muscles and support the repair.
- Diet and Nutrition: Maintain a balanced diet rich in fiber to avoid constipation, which can strain the pelvic area. Adequate hydration is also important for healing.
- Gradual Return to Work: Depending on your job and physical demands, you may be able to return to work within a few weeks. Discuss with your healthcare provider when it's appropriate for you to resume work activities.
- Sexual Activity: Your healthcare provider will provide guidance on when it's safe to resume sexual activity. This timeframe can vary depending on individual healing and comfort.
Lifestyle changes after Anterior Colporrhaphy Surgery:
After anterior colporrhaphy surgery, adopting certain lifestyle changes can help support your recovery, promote healing, and minimize the risk of complications. These changes are aimed at ensuring your pelvic area heals properly and maintaining overall well-being. It's important to follow your healthcare provider's suggestions and guidance for a successful recovery. Here are some lifestyle changes to consider:
- Rest and Recovery:
- Give your body adequate time to heal. Rest is crucial during the initial weeks after surgery.
- Avoid strenuous activities, heavy lifting, and intense exercise until you receive clearance from your healthcare provider.
- Pelvic Floor Exercises: Practice pelvic floor exercises (Kegels) as recommended by your healthcare provider. These exercises help strengthen the pelvic muscles and support the surgical repair.
- Hygiene and Wound Care:
- Follow proper hygiene practices to prevent infection. Keep the surgical area clean and dry.
- Avoid using harsh soaps or products that may irritate the surgical site.
- Diet and Nutrition:
- Maintain a balanced diet rich in fiber to prevent constipation, which can strain the pelvic area. Include fruits, vegetables, whole grains, and plenty of water.
- Adequate protein intake supports tissue healing. Consult your healthcare provider for dietary recommendations.
- Avoid Straining:
- Avoid activities that could strain the pelvic area, such as heavy lifting, pushing, or pulling.
- When using the restroom, avoid straining during bowel movements. You may use stool softeners if recommended by your healthcare provider.
- Proper Bowel Habits:
- Establish regular bowel habits to prevent constipation and minimize pressure on the surgical area.
- Stay hydrated and consume enough fiber to promote healthy bowel movements.
- Weight Management: Maintain a healthy weight, as excess weight can put additional strain on the pelvic area and surgical repair.
- Smoking and Alcohol:
- If you are a smoker, it would be beneficial to either quit or reduce your smoking habits. Smoking can hinder the healing process and also increase the likelihood of experiencing complications.
- Additionally, it's recommended to limit your alcohol intake as it can also interfere with the healing process and potentially interact with any medications you may be taking.
- Sexual Activity: Follow your healthcare provider's guidance on when it's safe to resume sexual activity. Allow sufficient time for healing before engaging in sexual intercourse.
- Follow-Up Appointments: Attend all scheduled follow-up appointments with your healthcare specialist. These appointments are necessary for monitoring your progress and addressing any concerns.
- Communication: Keep open communication with your healthcare provider. Report any unusual symptoms, changes, or concerns you may have during your recovery.